Happy Holidays fellow biodefense gurus! We at the Pandora Report would like to wish you and yours a lovely holiday season, filled with happiness, health, and a side of relaxation. Your favorite weekly dose of biodefense news be taking a few weeks off from reporting while I venture to the land of Oz. Rest assure, should there be a zombie outbreak, I’ll report it first hand! Since we’ll be radio silent for a couple of weeks, we’ve compiled a pretty swanky “I love biodefense and need more of it” reading list to keep you busy. Before you venture down the biodefense rabbit hole, here is fun history fact Friday: on December 24th, 1814, the war of 1812 ended and on December 24, 1936, the first radioactive isotope medicine was administered by Dr. John Lawrence.
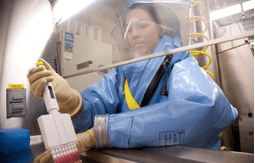
The Revolving Door of Biosafety
GMU Biodefense Master’s student and lab guru, Scott McAlister discusses the importance of biosafety in the changing world of global health. Through his review of the 2009 report by the Trans-Federal Task Force on Optimizing Biosafety and Biocontainment Oversight and a 2015 memorandum released by the White House to enhance biosafety, he discusses the ever changing components of US biosafety. Scott breaks down and compares each report’s recommendations, language, and what these translate to within US laboratories. Moreover, given the recent failures, have US biosecurity practices and recommendations evolved over the past 6 years? Take a look into this review to see where we hope to be and if we’ve progressed since 2009.
National Action Plan for Combating Multidrug-Resistant TB
This week the White House released its national plan for combating the growing threat of multidrug resistant tuberculosis. While US rates of TB cases have dropped, the growing threat of multidrug resistant TB (MDR-TB) and extensively resistant TB (XDR-TB) requires action. This new plan is set to span over 3-5 years and has three goals that will focus on strengthening domestic capacity, improving international capacity and collaboration, and accelerating basic and applied research and development. Extensive collaboration within US agencies and international partners will be necessary to combat the evolving threat of drug resistant tuberculosis.
We’re Not Prepared for a Biological Attack
GMU Biodefense PhD alum, Dr. Daniel M. Gerstein, discusses biopreparedness and where the US stands in his work for US News & World Report. Throughout his in-depth analysis, Dr. Gerstein emphasizes the importance of US leadership within the Biological Weapons Convention (BWC). Pointing to the disappointing Seventh and Eighth Review Conferences, Dr. Gerstein notes, “biological warfare can no longer be considered the purview of only state actors. And this democratization of biotechnology means that the world is literally one rogue microbiologist away from a potentially devastating biological attack.” Dr. Gerstein emphasizes that authorities often fail to realize that biological weapons may not act like naturally occurring diseases or outbreaks.
Holiday Biodefense Book Club
During the cold winter months it’s always nice to curl up by the fire with a good book and relax. GMU Biodefense Master’s student, Rebecca Earnhardt, and I have picked a handful of books to spark your interest. If we could have a book club with our awesome readers, we would love it, but in the mean time, here are our recommendations for a few literary works that you might enjoy!
- Phantom Menace or Looming Danger?: A New Framework for Assessing Bioweapons Threats By Kathleen M. Vogel — Johns Hopkins Press, 2012. The military has gathered reconnaissance of a possible biological research facility, evidence of a paper trail indicating procurement of weapons delivery systems, and collection of specialized personnel to manufacture biological agents. Do all of these pieces point to an imminent biological weapons danger? Kathleen M. Vogel, in Phantom Menace, argues that there is more to the picture of biological weapons development than the technical and physical aspects of manufacturing. Through examination of three case studies, Vogel highlights the shortcomings of the dominant biotech revolution frame within biological weapons assessments. The biotech revolution frame, as described by Vogel, misses the important social and contextual factors that affect biological weapons innovation. The alternative offered by Vogel is termed the biosocial frame. Vogel highlights in her biosocial frame how tacit knowledge and hands-on experience is vital to biological weapons assessments. While Vogel does not particularly focus on political influences, I enjoyed the book because of her explanation of the importance in incorporating sociological aspects into biological weapons assessments. I think this makes Vogel’s work a key book in the field of biodefense.
- Innovation, Dual Use, and Security: Managing the Risks of Emerging Biological and Chemical Technologies. Editor: Jonathan B. Tucker — MIT Press, 2012. The hotly debated concept of ‘dual-use’ is explored extensively through this multipart work edited by the late chemical and biological weapons expert, Jonathan B. Tucker. This book takes on the conceptual nuances of dual-use with four parts focused on emerging technologies within the areas of directed design, acquisition of novel molecular parts, modification of biological systems, and enhanced production and packaging capabilities. Each section, authored by leading experts in the field of biodefense research, including Filippa Lentzos and Gerald Epstein, applied Tucker’s framework of risk assessment for dual-use potential and governability. This framework incorporates key aspects of assessing dual-use potential, including technological monitoring, technology assessments, and governability of the technology. The strength of this framework lies in its applicability to emerging technologies, which may enable policy makers to continuously review a particular technology or an emerging area of research. In the concluding chapter, Kirk Bansak and Jonathan Tucker redirect attention to the intervening social processes that construct relationships between the technology and its users, and how these social processes may create an environment ripe for misuse. To me, this book is a highly valuable and informative work on the range of dual-use issues and conceptual applications. I think this book is an important read not only because it covers a variety of dual-use issues, but also in its wide-ranging review of relatively recent biotechnology and life science innovations. The variety of case studies makes this book an enjoyable read!
-
Spillover: Animal Infections and the next Human Pandemic by David Quammen. New York: W.W. Norton, 2012. Not only is David Quammen one of my favorites, but his overview of zoonotic diseases and the concept of spillover will both captivate and inform you. Ranging from West Nile Virus to Ebola, Quammen presents several of the zoonotic diseases you may have heard of and others that may cause you to reconsider kissing a horse anytime soon. Each chapter presents a new disease, it’s history, and a new outbreak that should raise our attention to global health security. While he doesn’t touch much on avian influenza or multi-drug resistant organisms, his points on humans infringing upon animal ecosystems and the resulting disease spillovers are harrowing. Quammen’s adventures remind me of a microbial Indiana Jones (hint hint Hollywood, that would make an excellent movie!), even with the cheeky wit. I would recommend Spillover as a gateway to understanding the role of zoonotic diseases and the emphasis we’re seeing on One Health. While his parts on Ebola aren’t as dramatic as Richard Preston, you’ll be sure to enjoy his approach to epidemiology and the impact of spillover on global health. Quammen did extend his sections on Ebola into another book that includes information related to the 2014/2015 outbreak. If you enjoy on-the-ground reporting, you’ll find this within Quammen’s book.
-
Greek Fire, Poison Arrows, and Scorpion Bombs: Biological and Chemical Warfare in the Ancient World by Adrienne Mayor. Woodstock: Overlook Duckworth, 2003. As a lover of all things biodefense and classical, I was excited when I cam across Adrienne Mayor’s book. Combining ancient history and bioweapons? Sold! Mayor’s breakdown throughout the book reveals the mythical and historical accounts of chemical and biological weapons in the ancient world. While a bit dramatic and sometimes repetitive, I found her book to be enjoyable in that few people have combined ancient history and chem/bioweapons to such an extent. Mayor makes sure to include references to mythology that heavily impact these ancient societies. While the lines of chemical and biological weapons were sometimes muddied and some generalizations related to classical history did occur, I would recommend her book to anyone who enjoys history (especially ancient history), mythology, and CBW. Realistically, with such a catchy title, how could you resist?
Stories You May Have Missed:
- Tracking Zebras and Barriers to Bioweapons – Dr. Amesh Adalja reviews GMU Biodefense Professor, Dr. Sonia Ben Ouagrham-Gormley’s Barriers to Bioweapons in his blog, Tracking Zebras. Discussing the role of tacit knowledge and the formative stages of development, Dr. Adalja’s experience as an infectious disease physician provides new insight into Dr. Ben Ouagrham-Gormley’s book.
- Bacteria Resistant to Last Drug of Choice Found in UK- bacteria that is resistant to colistin, the common antibiotic of last resort, has been found in the UK after it was identified in China last month. Ongoing monitoring and analysis is being done to track the gene (mcr-1) that allows bacteria to resist colistin and can potentially spread among species.
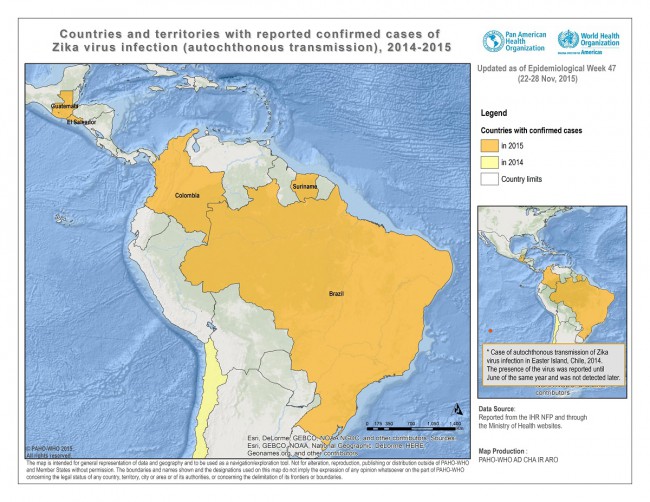
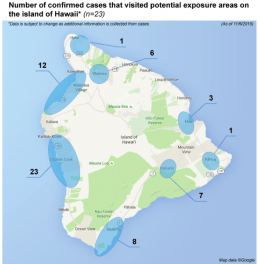
- Outbreak Updates: The Zika virus outbreak has now reached Cape Verde with over 4,700 potential cases and four cases have been identified in Panama. No new cases of Ebola have been reported this week! The Food and Drug Administration (FDA) is now joining up with the CDC since the second wave of Chipotle E. coli cases.