The Pandora Report is going on a brief hiatus. We’ll see you soon!
Category: News
ABSA 2021 Conference- Biosafety, Biosecurity, and Filling the Toolbox: Staying Vigilant and Preparing for the Next Public Health Event
By Emily Johnson, Biodefense MS Student
Introduction
The United States is experiencing a decline in COVID-19 cases, but SARS-CoV-2 is still a prominent topic here and internationally. The American Biological Safety Association’s (ABSA) 64th Annual Association for Biosafety and Biosecurity Conference took place October 25-27, 2021, bringing together a global community to discuss these topics while aiming to provide solutions to tackle the most challenging issues, present fascinating case studies, and showcase the latest developments in biosafety and biosecurity. The conference was presented virtually, offering a platform similar to a live conference including a lobby, exhibit hall, poster hall, networking lounge, and live presentations.
Overview of ABSA Virtual Conference Report
I attended this virtual conference along with my GMU Biodefense Program colleague, Mr. Konnor Heyde. To provide our readership with a comprehensive report on the ABSA conference, we self-assigned the sessions we would write about. This report provides an overview, details, and comments on the following sessions:
- Session I: Virology in the Time of a Pandemic
- Session III: The COVID Pandemic: The Evolving Reality
- Session XII: Gene Therapy
- Professional Development: Identifying and Overseeing Potential DURC: A practical Guide for the Biosafety Professional
Session I: Virology in the Time of a Pandemic
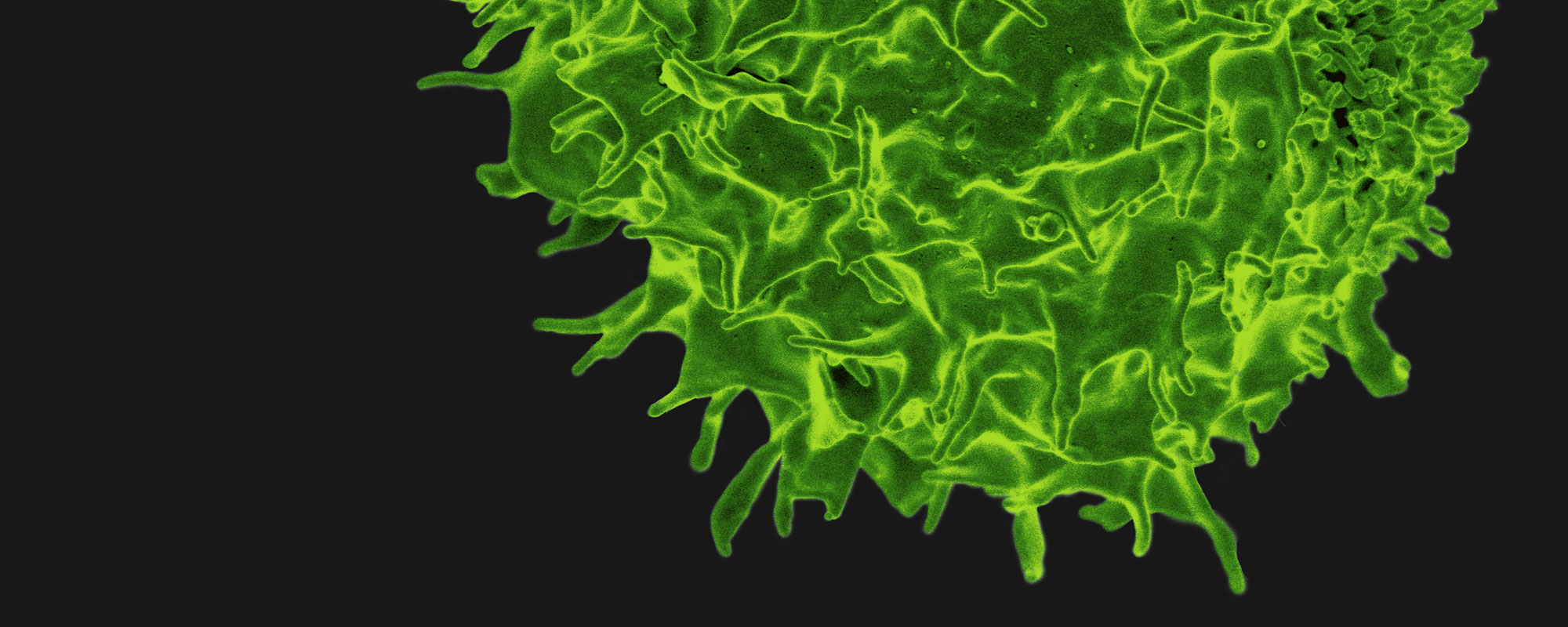
When a novel virus emerges in a population there is no substitute for preparedness in improving the effectiveness and timeliness of the response. The conference commenced with Dr. Dirk P. Dittmer from the University of North Carolina—Chapel Hill discussing the causative agent of COVID-19, testing, and disease outlook.
He began by utilizing a case study format, presenting an “old” pandemic: HIV. The progression of the pandemic was separated into three phases and compared to the current pandemic. It began with a phase he designated as “pre” which, for HIV, was before publication of the July 1981 MMWR report recognizing abnormal presentation of pneumonia in both San Francisco and New York. The rate of occurrence increased exponentially creating a bell curve which was the pandemic phase. The curve dropped precipitously, though never returning to zero even after effective treatment using antiretrovirals was approved. This was the transition to the “post” phase. For the COVID-19 pandemic, Dr. Dittmer defined the “pre” phase as the period leading up to the release of the article in the New England Journal of Medicine on A Novel Coronavirus from Patients with Pneumonia in China, 2019. Dr. Dittmer considers the pandemic phase as ending with the FDA approval of a vaccine in August of this year in addition to an EUA for other treatments.
The Global Initiative on Sharing Avian Influenza Data (more commonly known by its acronym- GISAID) is a worldwide repository of genomic sequences historically used to catalog international influenza variants. It played a critical role in the identification and tracking of emerging strains of SARS-CoV-2 variants. By March of 2020, the G614 variant was present in the US, exhibiting lower CT values (referring to the PCR cycle threshold where a florescent signal is first detectable) suggesting a higher viral load and therefore an increase in transmissibility over the wild type. This does not necessarily indicate more severe disease. In May 2021, the delta variant arrived in the US and, as of September, was indicated in over 90% of cases.
Dr. Dittmer referred to the pre-pandemic period as a time of blissful ignorance and squandered opportunities. He identified one failure as the self-imposed bottleneck by the single PCR test manufactured in a single place that slowed testing in the US. Another example of this is the underfunding of proposed basic science research on viruses related to HIV or SARS-CoV-2 prior to their respective outbreaks. Limited funding resulted in few experts on coronaviruses. The lesson to be learned is that while research will escalate during a pandemic, basic science research should be supported between public health emergencies.
Constant preparedness is crucial. Previous work on techniques to increase accuracy in virus detection resulted in a broad knowledge base from which researchers could build when faced with the testing demands of the COVID-19 pandemic. Plaque assays measure infectious virus, but they are time consuming. QPCR overestimates viral load because it includes viral segments. This means the CDC assay is more sensitive because it measures full genome as well as segments while the WHO assay only reports full genome.
Dr. Dittmer’s lab is using Rapid NextGen Sequencing methods. There is a linear relationship between viral load and number of reads, therefore it can also be used as a viral load assay, albeit an expensive one. It takes about 100,000 reads to determine a whole genome. The results suggest that most genomic material sequenced was whole genome, therefore eliminating the advantage of the CDC assay over the WHO assay.
NextGen sequencing can be used in fragment detection, even with a low number of reads. If the segments are dispersed throughout the target genome it is likely the fragmented virus was present in the sample. Although further testing is needed, he proposes a relationship between sequence coverage and infectivity. The higher the number of reads, the more likely the sample contained infectious virus. The remaining barrier is cost.
The next pandemic cannot be predicted. There is no magic bullet. The best way to prepare is to be ready for the unpredictable. This, Dr. Dittmer, says is the value of basic science.
Session III: The COVID Pandemic: The Evolving Reality
In 2005, Dr. Michael T. Osterholm published an article in the New England Journal of Medicine outlining the inevitability of an imminent pandemic and a strategy to prepare. These warnings went mostly unheeded. In this fireside chat, he discussed the state of the COVID-19 pandemic, posed questions to be investigated, and measures that should be taken to prepare not only for the next inevitable pandemic, but for the impending surges of COVID-19 the US is likely to continue to experience. He is a leading epidemiologist, director of the Center for Infectious Disease Research and Policy, professor at the University of Minnesota, and in November of 2020 was appointed to President-elect Joe Biden’s Transition COVID-19 Advisory Board.
Dr. Osterholm began by discussing the mystery of the four- to six-week surges in geographical hot spots of COVID-19 cases during which he draws parallels between this phenomenon and the 2009 H1N1 outbreak. At the beginning of that pandemic, there was a surge in cases during the March/April timeframe followed by a significant drop with no mitigation factors in place. This repeated in the late Fall. That winter, the cases of H1N1 were sparce, but more interestingly, there was an international phenomenon of a drop in seasonal flu cases. Similarly in 2020, all respiratory diseases appeared to decrease in prevalence. He observes that this is not the result of human action as it was equally demonstrated in countries with and without mitigations.
The Dawn of the Age of the Variants
In November 2020, the SARS-CoV2 alpha variant was detected in the UK. It was this point where he said his analogy changed from which inning of the COVID-19 pandemic baseball game we were in to how many minutes of the game had passed. Variants can be associated with changes in transmissibility, severity, or the ability to evade natural defenses and vaccine immunity. There is potential for emergence of novel variants as the pathogen continues to spread. With 65 million eligible Americans still unvaccinated and Russia experiencing an uptick in cases due to similar hesitancy among the Russian population to accept the Sputnik vaccine, we have a population ripe for the spread of this virus for months or years to come. However, Dr. Osterholm believes that COVID-19 is likely to present seasonally in the future.
Another point where SARS-CoV-2 is not analogous to seasonal influenza is that when a pandemic influenza becomes a seasonal virus, it attenuates into a seasonal pattern and genetic changes are unlikely to result in it becoming more challenging. Conversely, we do not know what severity or transmissibility modifications future SARS-CoV-2 variants will exhibit.
Vaccines: Study, Learn, Implement, Repeat
When mRNA data was originally released, it showed high rates of safety and over 90% protection from severe illness, hospitalization, and death. The Johnson & Johnson adenovirus-based vaccines showed lower initial immune response, only reaching about 74%.
The mRNA vaccines exhibit waning immunity over time. It is still unclear what this will mean over the long term, but he predicts break through cases will continue to increase in number and in younger populations as they received their initial vaccine later than the older population and are now reaching a valley of immunity.
Dr. Osterholm believes the adenovirus-based vaccines will be the game changers with COVID-19. Although the mRNA vaccines initially reached a higher rate of protection, it dropped over time while the Johnson & Johnson vaccine improved over time, reaching the low 80% range by six months post-immunization. A second dose increases numbers into the 90% range, and this may be more enduring. We must learn how to best use these vaccines concerning mixing, dosing, and timing. There may be multi-strain vaccines in the future, but improvements seen in second or third generation COVID vaccines will likely be developments related to temperature tolerance and, possibly, coverage for variants.
Laboratory Safety
During his tenure on the Natural Science Advisory Board for Biosecurity, he was very critical of the research on mammalian transmission of H5N1, citing his respect for the importance of laboratory and biologic safety issues. He views the origins of SARS-CoV-2 in a similar light and is concerned with lab safety. However, he believes that while it is possible the virus originated in a lab, it is likely the result of a spillover event like SARS or MERS. He went on to point out that Wuhan is a transportation hub in China with millions of travelers traversing the city daily. In addition, there is a thousand-mile reach for food, particularly live animals, coming to the markets of Wuhan. This evidence supports a spillover scenario. He dismissed the cleavage site evidence of a human-manipulated genome citing similar genetics in coronaviruses found in caves in Laos.
To demonstrate his point, he proposes the hypothetical situation of a novel virus emerging in the Caribbean. One of the initial regions the virus would be clinically detected is Atlanta, Georgia due to it being a transportation hub between North America and the Caribbean. Would the international population assume the virus escaped from a CDC lab?
Question & Answer Session
When asked why there were more cases in the US than China where it originated, Dr. Osterholm was quick to point out that those two elements are not related. China imposed draconian quarantine measures and rampant testing while the US has not. There are many factors contributing to the respective countries’ reported number of cases.
Another attendee asked why immunity from infection was not equal to that of the vaccine. Dr. Osterholm explained that we do not fully understand what immunity to COVID-19 is yet. In the first weeks after mRNA vaccination, study participants showed high levels of protection from disease, but almost undetectable antibody levels. Cellular immunity was playing some role in that protection that is not yet fully understood. There is conflicting data on what immunity is offered by natural infection. While it does afford some protection, how good it is and how long it lasts are still unknown. There is strong evidence that those who receive a vaccine after natural infection are at a lower risk, similar to the natural infection acting like a first dose.
A question asked by many since the pandemic began is, “What could have been done differently in the beginning?” He replied that not much can be done once a respiratory virus establishes itself in a population. There is no magical solution. The US could have improved in preparations for a major health event. A better prepared healthcare system will be integral in successful navigation of future pandemics. He also cited improving communication with the public.
Lastly, he believes there is a zero chance of eradication. It is more likely that with long-term vaccination, COVID-19 will eventually present in a seasonal manner like influenza.
Session XII: Gene Therapy Research Boom and Future Challenges
Dr. Daniel Eisenman of Advarra shared an overview of the progression of gene therapy research and the changes relevant to an institutional biosafety committee.
To review the process of regulatory oversight of gene therapy research, it begins with preclinical research and development involving only animal models. When potential has been shown, an application for an Investigational New Drug (IND) is submitted to the FDA. Phase two is the first clinical phase involving humans. It usually involves 20 to 100 subjects, although Dr. Eisenman pointed out that the trial for a COVID-19 vaccine had around 30,000. The focus of phase two is to prove safety. In phase three, the focus shifts to showing efficacy, it involves more participants, and it has determined optimal dosing. After successfully completing phase three, FDA approval is requested. Phase four includes post approval research.
Immediately preceding the pandemic, Dr. Eisenman published an article in Applied Biosafety which demonstrated the dramatic, explosive growth in the number of gene therapy IND applications per year. By 2020, that number had flatlined. Why? As a result of COVID-19, many clinical trials were suspended.
Prior to COVID-19, most gene therapy submissions were for oncological application. Now, among the most recent approvals, there were eight for oncology, but six for infectious diseases (two of which were COVID-19 vaccines) and two for rare diseases. These successes pave the way for future therapies.
Two gene therapy success stories were presented. The first was treatment for retinitis pigmentosa, a disease characterized by night blindness at a young age that progresses to total blindness. The therapy reversed vision loss demonstrated by the speed with which they were able to navigate a dimly lit maze. The other example of a successful application was treatment of spinal muscular atrophy type 1. SMA1 usually results in death during toddlerhood due to the inability to control muscles involved in breathing. Children who have undergone treatment are living into childhood and are even able to walk and run on their own.
There are currently over 350 gene therapies in phase three trials. In a recent statement on advancingthe development of safe and effective cell and gene therapies, the FDA suggested that gene therapy may be at a turning point similar to that of monoclonal antibodies in the late 1990s. The technology has the potential to become a backbone of modern treatment regimens.
Dr. Eisenman then went on to discuss some changes in Institutional Review Board (IRB) involvement in multi-site studies. Traditionally an IRB review is done at each institution where the clinical trial is being carried out. This can be inefficient. As of 2018, all NIH funded multi-site studies are required to utilize a single IRB. Other federally funded studies made the change in 2020.
NExTRAC is the Novel and Exceptional Technology and Research Advisory Committee. It no longer oversees individual clinical trials but instead relies on prompts which would direct public deliberation on certain research. This is one result of the burden of oversight shifting from NIH to the FDA.
One recommendation Dr. Eisenman hasd is for the public to request more formal FDA requirements for shedding data during clinical trials. Currently it is risk based and more of a recommendation as FDA exemptions are regularly requested and granted. He suggested it should be included for all vector-based studies and replication-competent microbes, including vaccines.
Conclusion
The presentations shared at the conference were very informative, thought provoking, and had a general feeling of collegiality from living the pandemic and experiencing similar struggles. One of the presentations exhibiting ingenuity resulting from COVID-19 was given by Benjamin Fontas. He discussed the development of Short Term Use Biocontainment Bubbles at Yale (STUBB-Y) where researchers drew on their expertise to provide professionals working in high risk occupations at Yale temporary protection from aerosols at the beginning of the pandemic. This was just one example of the innovative applications of biosafety experience that presenters contributed to their institutions to mitigate safety concerns during the pandemic.
COVID-19 vaccines were also discussed by multiple speakers, specifically regarding the need to look at them as one of the tools in our toolbox, not a final solution. A recurrent theme was the importance of communication with the public to ensure their trust in science and scientific representatives. From misinformation about mitigations to questions about the ability of novel pathogens to escape a lab, it is more important now than ever that the public is communicated with in a way that encourages trust and understanding.
Professional Development Course on Dual Use Research of Concern
Professional development courses were offered in conjunction with the ABSA 2021 conference. I attended Identifying and Overseeing DURC: A practical Guide for the Biosafety Professional presented by Rebecca Moritz, Biosafety Director at Colorado State University.
Dual Use Research of Concern (DURC) is defined by the National Institutes of Health (NIH) as “life sciences research that, based on current understanding, can be reasonably anticipated to provide knowledge, information, products, or technologies that could be directly misapplied to pose a significant threat with broad potential consequences to public health and safety, agricultural crops and other plants, animals, the environment, materiel, or national security.” It is interesting to note there is a difference between dual use research and dual use research of concern. They both refer to research that could be used for both beneficial and malevolent purposes. However, DURC directly references a significant threat with broad consequences.
Historically relevant cases of DURC include the mousepox experiment by Jackson et. al in 2001 and the 1918 influenza research by Tumpey in 2005. In 2004, the National Academies of Sciences released Biotechnology Research in an Age of Terrorism, better known as the Fink Report. The goal was to better educate the scientific community on how their research could have unintended consequences.
To better guide those defining what should be considered concerning research, the National Science Advisory Board for Biosecurity released the Proposed Framework for the Oversight of Dual Use Life Sciences Research: Strategies for Minimizing the Potential Misuse of Research Information. The guiding principles focused around oversight that would maintain public trust by demonstrating that the scientific community recognizes potential security threats and is acting responsibly to protect the public safety and security. However, it cautions that there must be a balance that allows for both oversight and research advancement.
Similarly, research on potential pandemic pathogens (PPPs) is necessary to protect global health and security. The Department of Health and Human Services released the Framework for Guiding Funding Decisions about Proposed Research Involving Enhanced Potential Pandemic Pathogens (P3CO) in 2017. This framework guides department-level pre-funding review on research that may create, transfer, or use enhanced PPP.
The most recent DURC policy went into effect in 2015. The framework should be applied in cases that involves one of the 15 agents listed in the policy or if it has the potential to result in one of the seven experimental effects listed. This includes enhancements in consequences, resistance, or transmissibility, disrupting immunity, altering the natural host range, or reconstituting an extinct agent. Interestingly, the reference to a “novel pathogen” was dropped between the 2012 and the 2014 versions, but it is still a topic to be taken into consideration. In fact, it is possible for research outside the scope articulated in the policy to still be DURC and require review.
The Institutional Review Entity (IRE) board performs a risk assessment on any research or work done at the institution that is subject to DURC evaluation. The members should have sufficient expertise to assess dual use of a range of scenarios but may also contact consultants as needed. These plans, including mitigations, should be reviewed annually.
There are many points to consider when reviewing the whole lifespan of proposed research for DURC. They can be summarized by looking at how the work will be performed and results communicated, the scope of consequences with countermeasures taken into consideration, the potential timeframe for misuse, and the skill, knowledge, or technology needed to use the product for nefarious purposes. Potential benefits are also an essential aspect of the review. DURC should not be only associated with the unscrupulous application of science. The goal is knowledge or methods that will benefit humanity. If there are risks, it is important to consider if they target a specific population.
Recognizing a risk is present is not necessarily reason to deny the research from proceeding. Risk mitigation can reduce the risk to a level that is acceptable when compared to the potential benefits. These plans may include biosafety, biosecurity, personal protective equipment, standard operating procedures, occupational health plan like vaccines, training, and countermeasures. Institutions may apply varying mitigations as appropriate for each individual situation.
If existing measures are not adequate to mitigate conceivable risk, creating a mitigation plan may be the means to receive funding from a government source. Subsequently ensuring compliance with the plan is essential. One way to encourage this is by the IRE maintaining a positive relationship with the primary investigator and requesting that they report any changes that may alter the evaluation. Another source that may assist in identifying DURC is the institutions’ grant administrators. These mitigation plans may be subject to Freedom of Information Act requests and therefore should not disclose institutional proprietary or security information.
To close the session, dual use case studies were presented and evaluated. This was a learning opportunity to practice what had been taught, but also to experience how subjective interpretations can be. Those same case studies were used to develop risk mitigation plans that would alleviate the most pressing risks while still allowing the research to take place and be submitted for publishing, possibly with some changes.
Pandora Report: 1.7.2022
Happy New Year from the Pandora Report! We hope everyone had a jolly and healthy holiday season! January is One Health Awareness Month to promote the approach of greater cross-sectoral collaboration and communication across the human-animal-environment interface. In big news, Danyale C. Kellogg, a Biodefense PhD student, is taking over as the Managing Editor of the Pandora Report and we cannot wait to see more of her insights and expertise.
Remembering Stephanie Smith
The Biodefense Graduate Program is sad to report the recent passing of alumna Stephanie Smith (MS ’17). Stephanie had a love of science, boundless curiosity, a keen mind, and engaging personality. She made the most of her time in the program and in her role as the Science and Technical Advisor to the US Postal Inspection Service she exemplified the Biodefense program’s ideal of bridging the gap between science and policy. The Biodefense Program offers her family and friends our deepest condolences.
January Is One Health Awareness Month!
To promote collaboration between animal, environmental, plant and public health scientists, on December 19, 2019 the US Senate unanimously passed a bipartisan Senate Resolution 462 (S Res 462) introduced by Senators Dianne Feinstein (Democrat-California) and Martha McSally (Republican-Arizona) designating January 2020 as “National One Health Awareness Month” in the US. Excitingly, the campaign was picked up and promoted by One Health advocates around the world. Help keep the momentum going! To help spread the word, you can use the hashtags #OneHealth and #OneHealthAwarenessMonth!
3 Issues to Watch in Global Health in 2022
As we enter the third year of COVID-19, STAT has identified three issues in the world of global health and infectious diseases that are worth keeping an eye on. (1) Will 2022 be the year Covid starts to settle down, to show signs of being more endemic, less pandemic? This year, COVID-19 vaccine doses should become more widely used in lower income nations. But, will these vaccines need to be updated to better combat the emerging variants? (2) What will happen with the World Health Organization (WHO) this year? The WHO has come under much scrutiny the last couple years, and funding has been a struggle. Also, the World Health Assembly will soon vote on whether to give Tedros another five years at the helm. (3) How will vaccination rates fair in 2022? Lower income countries have struggled to get their hands on enough doses, but that will hopefully change in 2022. On the other hand, the US has seen great opposition to COVID-19 vaccine mandates and many are still unvaccinated.
10 Key Global Health Moments From 2021
The World Health Organization (WHO) shared 10 global highlights from 2021 ranging from innovation in vaccines to inequities in vaccine distribution, but also a new malaria vaccine and a drop in tobacco use. The COVID-19 pandemic has continued to strain the health systems of nations in conflict, such as Yemen and Syria. The WHO states that the pandemic is “likely to halt two decades of global progress towards universal health coverage (UHC), having triggered the worst economic crisis since the 1930s and badly disrupted health services.” Health systems overcoming the challenges of 2021 are doing so in large part thanks to the “huge sacrifices of the women who represent 70% of the health and social workforce.” 2021 marked the 100th anniversary of the discovery of insulin and the WHO launched a Global Diabetes Compact to “speed up action on the prevention and treatment of diabetes.” Read more here.
Multi-Service Tactics, Techniques, and Procedures for Domestic Chemical, Biological, Radiological, and Nuclear Response
This publication provides doctrinal guidance for executing domestic chemical, biological, radiological, and nuclear CBRN response operations under the auspices of defense support of civil authorities (DSCA) and describes Department of Defense (DOD) roles and responsibilities in conducting domestic CBRN responses. It also describes the framework for domestic response, operational fundamentals, and DSCA.
Chapters are oriented around DOD support for domestic CBRN incidents as a component of the National Response Framework (NRF) to provide organizational understanding and knowledge of response activities in support of a domestic CBRN response. The publication contains appendixes that present additional details on specific domestic CBRN response organizations and their associated capabilities and selected related topics. This publication reflects changes in the capabilities within the CBRN response enterprise and recent changes in associated guidance, methodology, and terminology.
Chapter 1 provides an overview of the national frameworks for US domestic response. Chapter 2 focuses on initial planning and anticipation of CBRN incident response and activities, in line with the CBRN response phases of shape and anticipate. Chapter 3 focuses on the phases of respond and operate. Chapter 4 focuses on the phases of stabilize and transition. Read the publication here.
CBRN Terrorism Interdictions (1990–2016) and Areas for Future Inquiry
The pursuit and use of chemical, biological, radiological, and nuclear (CBRN) weapons has been examined by scholars for more than two decades. What has not been examined are the cases in which non-state actors were prevented from obtaining or using these weapons and agents and the corresponding reasons for successful interdiction. This article uses the Profiles of Incidents Involving CBRN and Non-State Actors (POICN) database to carry out an exploratory analysis of CBRN interdictions around the world from 1990–2016. Using basic descriptives and cross-tabulations, this study finds that successful interdictions often resulted from probable cause searches, surveillance operations, but also from other, unknown reasons. However, there is a tremendous amount of variation when it comes to modes of interdiction and actor motivation. The same goes for jurisdiction, whether international collaboration aided the interdiction, and weapon acquisition and delivery. This text is intended to serve as a foundation for the study of CBRN terrorism interdiction as it seeks to undercover why some law enforcement efforts fail while others succeed. The author, Dr. Wesley D. McCann, is an Assistant Professor in the Department of Criminology, Law and Society at GMU. Read the article here.
A Handbook for Ending Catastrophic Biological Risks: How the United States Can Prevent Future Pandemics and Deter Biological Weapons
In a time of daily confusion in the public discourse on the current pandemic, the Janne E. Nolan Center on Strategic Weapons, an institute of the Council on Strategic Risks (CSR), is releasing A Handbook for Ending Catastrophic Biological Risks: How the United States Can Prevent Future Pandemics and Deter Biological Weapons. Authored by some of the nation’s top experts in combating biological risks, this unique guide presents a “clear, viable and improved path” toward addressing them. It calls for a US government surge of investments in addressing biological threats of all origins, with detailed recommendations for improving US government programs and cooperative partnerships.
The Handbook for Ending Catastrophic Biological Risks starts with a bold, moonshot-level vision that can drive transformative changes—not the incremental improvements the US government has often pursued in the past. That vision has two critical parts:
The Handbook promotes an ideal yet achievable vision on naturally-arising biological risks: preventing future pandemics – moving beyond simply enduring them and accepting the lives lost and damage to health security, national security, and the economy that pandemics can cause.
The Handbook also details a complementary vision regarding deliberate biological risks (one which will require far more significant shifts in the nation’s goals and policies), asserting that: The United States should lead the world in making biological weapons the first category of weapons of mass destruction to be effectively eliminated or rendered obsolete. To advance this vision, the report recommends that national security leaders adopt a deterrence by denial strategy that focuses on denying an attacker success in their likely aims regarding biological weapons, such as causing mass casualties, mass confusion, and erosion of operational capabilities.
Dr. Yong-Bee Lim, recent graduate of the Biodefense PhD program, is among the authors of The Handbook. Find The Handbook here.
Second WHO Consultative Meeting on a Global Guidance Framework to Harness the Responsible Use of Life Sciences
On 7 September 2021, 47 participants attended the second World Health Organization (WHO) consultative meeting on the development of the global guidance framework to harness the responsible use of life sciences. Participants were drawn from all six WHO regions and brought a wide range of expertise, representing academia, scientists and researchers, publishers and editors, public health officers, policymakers, research donors, and representatives from regional and United Nations entities.
The objectives of the meeting were to discuss the findings and recommendations of the three working groups, which were established as a follow-up activity of the first consultative meeting held on 11 March 2011. In addition, participants were invited to discuss the next steps in the development of the global guidance framework to harness the responsible use of life sciences (the Framework). Finally, this meeting was intended to pursue the consultation and engagement processes on this area of work.
Participants welcomed and supported the findings and recommendations of the three working groups. The set of guiding values and principles underpinning the Framework was adopted and common understanding was reached on tools and mechanisms for governance and awareness raising, education, capacity building and engagement activities. It was agreed to link and cross reference the three documents developed by the working groups, noting the need for consistent language and terminologies across the three documents. The comprehensiveness of these documents was highlighted along with the need to have a practical and actionable Framework, which would refer to the current working groups’ themes.
Future activities include the development a glossary of key terminologies and the work on a series of case studies and scenarios to test the utility of the Framework and to demonstrate how the different elements of the Framework could be used in real and hypothetical situations. Two working groups will be established to carry out these activities. WHO will continue to consult with relevant individuals, groups, Member States and the regions on the development, dissemination and implementation of the Framework in the coming months. Read the report here.
ALL THINGS COVID-19
The Latest on Omicron
The Omicron variant of SARS-CoV-2 is spreading more easily than the original virus, but it “likely carries a lower chance of getting seriously ill.” There is preliminary evidence that the “risk of being admitted to the hospital or the intensive care unit during the omicron surge in the US is about half of the risk observed during the delta surge.” According to Dr. Pamela Davis, who’s a pulmonologist at Case Western Reserve University, “in the older age group, it’s still a nasty disease, even if it’s less [nasty] than the delta variant.” Now, in the US, there are 126,000 hospitalizations and more than a quarter of ICU beds are filled by COVID-19 patients. A recent study showed that vaccination reduces a person’s risk of severe illness and hospitalization.
Dr. Eric Topol provides an easy-to-follow overview of the Omicron variant of COVID-19, including how the vaccines combat this variant. Topol states, “while we have a very smart immune system that is vaccine- trained to defend surprisingly well against severe disease by a hyper-mutated, hyper -transmissible virus, too many humans have not gotten on board. We’ll nevertheless win this battle, fortunate to have 2 major points in our favor.”
700 Sheep and Goats Were Arranged in the Shape of a Syringe to Encourage Vaccinations
South of Hamburg, Germany, 700 sheep and goats were arranged into the shape of a 330-foot syringe. Shepherd Wiebke Schmidt-Kochan spent several days practicing with her animals to create the syringe as encouragement for people who are still hesitating to get vaccinated. In Germany, 71.2% of the population has received at least two shots and 38.9% has received a booster shot.

The US COVID-19 Vaccination Program at One Year: How Many Deaths and Hospitalizations Were Averted?
Nearly 800,000 Americans have died so far during the US COVID-19 pandemic, with more than half those deaths occurring during 2021. One year into the US vaccination effort, much attention has focused on the stubborn persistence of the pandemic, which has been fueled by new, more- transmissible variants and the millions of Americans who have not gotten their shots. However, the positive impact of the rapid development and deployment of highly effective vaccines — the reduction in deaths and hospitalizations — has been less obvious.
In July, The Commonwealth Fund reported that the US vaccination program had averted 279,000 deaths and 1.25 million hospitalizations, primarily by blunting a surge in the Alpha variant during spring 2021. Since that report, nearly all of the US has experienced a wave of infections, hospitalizations, and deaths caused by the highly transmissible Delta variant. More than 1,000 Americans are dying each day.
In an updated report, The Commonwealth Fund updates its estimates, through the end of November 2021, of COVID-related deaths and hospitalizations avoided because of the US vaccination program. Briefly, the agent-based computer model analyzes features of the coronavirus, its transmission, and its effects to compare the observed pandemic trajectory (infections, hospitalizations, and deaths) to a counterfactual scenario in which no vaccination program exists. The model incorporates the transmission dynamics of previous variants other than Omicron, which is only now beginning to appear in the US. The model accounts for waning immunity and changes in population behavior over time as schools and businesses have reopened and travel has increased.
In the absence of a vaccination program, there would have been approximately 1.1 million additional COVID-19 deaths and more than 10.3 million additional COVID-19 hospitalizations in the US by November 2021. Without the US vaccination program, COVID-19 deaths would have been approximately 3.2 times higher and COVID-19 hospitalizations approximately 4.9 times higher than the actual toll during 2021. If no one had been vaccinated, daily deaths from COVID-19 could have jumped to as high as 21,000 per day — nearly 5.2 times the level of the record peak of more than 4,000 deaths per day recorded in January 2021. Read the full report here.
17 Pandemic Innovations That Are Here to Stay
POLITICO asked its reporters to “identify the pandemic-induced policy innovations that have changed life in America over the last year and a half.” Following are a handful of the ways that the pandemic “spurred innovation in America, mostly for the better”:
- Cocktails-to-go
- Telehealth
- mRNA vaccines
- Robot deliveries
- “Warp speed” government investing
- “Streateries”
10 Lessons I’ve Learned From the COVID-19 Pandemic
STAT writer Helen Branswell looks back on the COVID-19 pandemic thus far and highlights 10 lessons learned from the last two years. The first is the “you gotta act fast,” especially in an outbreak of a novel pathogen. In early 2020, the world had hesitated too long and lost its chance to quickly contain the virus. Another hard lesson is that “even in the face of a deadly pandemic, politics override public health.” The pandemic showed that “political leaders [will] put the lives of their citizens at risk by downplaying or downright lying about a disease outbreak, just because telling the truth might jeopardize their political fortunes.” Much of the US response to COVID-19 has been “broken down along political lines.” This is exemplified by the lower vaccine rates red counties versus blue. Read more about COVID-19 lessons learned here.
Department of Defense Contributions to the US COVID-19 Response, at Home and Abroad
The US Department of Defense (DOD) should be systematically incorporated into any US government vision on international global health security. The United States should build on what has been learned and achieved through DOD support at home to the civilian-led COVID-19 response, as well as past DOD contributions to pandemic response overseas, and incorporate long-standing DOD international capabilities against biological threats. DOD should contribute to responding to the acute phase of the pandemic and build long-term preparedness capacities.
DOD has considerable assets in three areas that can and should be included, when appropriate, to support the US civilian-led international response:
- Logistics, lift, and planning;
- Biosurveillance and infectious disease research and development; and
- Relationships built through decades of international collaboration in biosecurity and biosafety, ongoing global health engagements, and work in overseas laboratories.
DOD already is playing a significant role in the procurement and delivery of 1 billion doses of the Pfizer-BioNTech vaccine, which President Biden has pledged to the COVAX vaccine solidarity mechanism to benefit 92 low- and lower-middle-income countries. A process of strategic planning for other likely DOD contributions to contain the global COVID-19 pandemic should begin right away. Read the full commentary from the Center for Strategic and International Studies (CSIS) here.
COVID Helped Cause the Biggest Drop in US Life Expectancy Since WWII
The pandemic has helped take 1.8 years off the average life expectancy for Americans in 2020, based on the latest federal mortality data. This marks the greatest change in the average American lifespan since World War II. In 2020, COVID-19 was the “third-most common cause of death in the United States, with one out of 10 fatalities due to the virus.” Dr. Zinzi Diana Bailey, a social epidemiologist at the University of Miami’s Miller School of Medicine, said, “A loss of two years seems limited, but that’s rolling back decades and decades of progress.” Death rates increased for all people aged 15 years or older in 2020. Though people ages 85 years or more died more frequently than the other age groups, people aged 35-44 years saw the biggest increase in death rates. One spot of good news is that the national infant mortality rate dropped 2.9%, a record low according to the Centers for Disease Control and Prevention.
EVENTS
Online International Symposium: COVID-19 Under the Pandemic Mass Gathering Events and Public Health Measures
When holding a mass gathering event represented by a large-scale international event such as the Olympic Games, it is necessary to prepare and respond to various risks. Japan has experienced many large international mass gathering events. In Japan, the focus has been on securing emergency medical care and mass disaster systems for such events, but in recent years there has been increasing interest in public health crisis management systems for infectious diseases and the like. The outbreak of the SARS-CoV-2 pandemic provided an opportunity to draw attention to the public health crisis management system in mass gathering. In addition to ensuring the safety of event participants, mass gathering is also required to be prepared to have a negative impact on the local health and public health system. The purpose of this symposium is to look back on the measures against mass gathering in the pandemic disaster and to obtain suggestions for future measures against mass gathering and measures against new coronavirus infectious diseases. This Zoom webinar will be held on 13 January. Register here.
Pandora Report: 12.17.2021
Congratulations to our new graduates: Dr. Henry Kim, Bianca Cruz, Nathaniel Morra, Deborah Cohen, Stephanie Clute, and Ashley Gonzalez-Bunce! The Pandora Report will be taking the holidays off – we wish you and your loved ones a happy holiday and wonderful New Year! We will see you again in 2022!
Congratulations to the New Graduates of the Biodefense Graduate Program!
This month, 6 students the Biodefense Graduate Program are graduating! Congratulations to newly minted Dr. Henry Kim! Congratulations to Bianca Cruz and Nathaniel Morra on graduating with the MS in Biodefense! Congratulations to Deborah Cohen, Stephanie Clute, and Ashley Gonzalez-Bunce for completing the certificate program! We wish you the best in your future professional endeavors! To all alumni, please stay connected by clicking here.
Army Training Emphasizes the Importance of Education in Preventing Chemical and Biological Attacks
Danyale C. Kellogg, a PhD student in the Biodefense Program, recently attended the Medical Management of Chemical and Biological Casualties course (MCBC), offered by the US Army Medical Research Institute of Chemical Defense (USAMRICD) and the US Army Medical Research Institute of Infectious Disease (USAMRIID) at USAMRICD’s facility in Edgewood, MD. She learned from instructors at these two legendary institutions how to identify chemical and biological warfare (CBW) agents, diagnose the conditions they cause, and mitigate their impacts. Upon applying to the Biodefense PhD program at the Schar School of Policy and Government at George Mason, she could not have predicted that during the first semester of she would be cutting a classmate out of Mission Oriented Protective Posture (MOPP) gear in the Maryland woods as part of a hands-on training exercise. This course was an incredibly informative, fascinating, and fun opportunity that was an excellent supplement to my graduate education. As an aspiring scholar-practitioner, understanding how the boots-on-the-ground manage these types of events and how such an event could impact broader operations and foreign policy is invaluable. Read about Kellogg’s takeaways here.
Jaime Yassif on Safeguarding Bioscience to Prevent Catastrophic Lab Accidents and Bioweapons Development
If a rich country were really committed to pursuing an active biological weapons program, there’s not much we could do to stop them. With enough money and persistence, they’d be able to buy equipment, and hire people to carry out the work. But what we can do is intervene before they make that decision. A recent guest on the 80,000 Hours Podcast with Rob Wiblin, Jaime Yassif — Senior Fellow for global biological policy and programs at the Nuclear Threat Initiative (NTI) — thinks that stopping states from wanting to pursue dangerous bioscience in the first place is one of our key lines of defense against global catastrophic biological risks (GCBRs). Links to learn more, summary and full transcript. It helps to understand why countries might consider developing biological weapons. Jaime says there are three main possible reasons: (1) fear of what their adversary might be up to; (2) belief that they could gain a tactical or strategic advantage, with limited risk of getting caught; and (3) belief that even if they are caught, they are unlikely to be held accountable. In response, Jaime has developed a three-part recipe to create systems robust enough to meaningfully change the cost-benefit calculation. The first is to substantially increase transparency. If countries aren’t confident about what their neighbors or adversaries are actually up to, misperceptions could lead to arms races that neither side desires. But if you know with confidence that no one around you is pursuing a biological weapons program, you won’t feel motivated to pursue one yourself. The second is to strengthen the capabilities of the United Nations’ system to investigate the origins of high-consequence biological events — whether naturally emerging, accidental or deliberate — and to make sure that the responsibility to figure out the source of bio-events of unknown origin doesn’t fall between the cracks of different existing mechanisms. The ability to quickly discover the source of emerging pandemics is important both for responding to them in real time and for deterring future bioweapons development or use. And the third is meaningful accountability. States need to know that the consequences for getting caught in a deliberate attack are severe enough to make it a net negative in expectation to go down this road in the first place. But having a good plan and actually implementing it are two very different things, and today’s episode focuses heavily on the practical steps we should be taking to influence both governments and international organizations, like the WHO and UN — and to help them maximize their effectiveness in guarding against catastrophic biological risks. Jaime and Rob explore NTI’s current proposed plan for reducing global catastrophic biological risks. Listen to this podcast here.
Dr. Brian Mazanec Featured on FedScoop Podcast
Dr. Brian Mazanec, an alumnus of the Biodefense Graduate Program and a Schar School adjunct professor, serves as the Director of Defense Capabilities at the Government Accountability Office (GAO) and was interviewed on the FedScoop podcast on 13 December about the government’s security clearance process. The clearance process has been on GAO’s High-Risk List since 2018. In a newly released report from the GAO, Personnel Vetting: Actions Needed to Implement Reforms, Address Challenges, and Improve Planning, evaluates the extent to which personnel vetting processes have implemented a reform based on the Security, Suitability, and Credentialing Performance Accountability Council (PAC) Principals. This report recommends that Congress consider requiring the Director of National Intelligence (DNI) to develop performance measures for continuous evaluation. GAO also recommends that that DOD revise the National Background Investigation Services (NBIS) schedule to fully meet the characteristics of a reliable schedule and establish a milestone to complete strategic workforce planning. Listen to the episode here.
Congress Passes Defense Policy Bill
The fiscal year 2022 National Defense Authorization Act will allocate $768 billion to the national defense budget and mandate a number of policy changes within the Department of Defense. The bill is now awaiting the signature of the president, and it is expected to be signed into law before the end of 2021. This legislation was passed by the Senate in a vote of 89-10 on Wednesday, and passed by the House earlier this month with a 363-70 vote. A Biden administration proposal would “cut spending on Defense Department programs that detect and counter diseases, even as COVID-19’s US death toll exceeds 800,000 people.” Under both the Biden and Trump administrations, the Pentagon has “asked Congress to scale back funding for the Biological Threat Reduction Program, despite successes that include funding a lab in Thailand that in January 2020 first detected the coronavirus outside of China.” Funding for the Chemical and Biological Defense Program, which works on the development of “everything from vaccines to protective suits” has also contracted. The Chemical and Biological Defense Program also helped Swine flu therapeutics, a vaccine for the Ebola virus and supported Operation Warp Speed. The National Defense Authorization Act would “add money above Biden’s requested amount for both of these programs. But appropriators, who provide the funds, are divided about how much to spend.”
Public Health Forward: Modernizing the US Public Health System
Public health serves a critical yet often invisible role in health. Although a disproportionate amount of attention is placed on medical care and the treatment of diseases, illnesses, and injuries, public health takes a communitywide approach to improving health and the social factors that contribute to good health. Healthy behaviors, social and economic factors, the physical environment, and other issues account for 80% of health outcomes, while clinical care is responsible for only 20%. Through such activities as promoting healthy eating and active living, controlling infectious disease outbreaks, and preventing injuries, public health efforts allow Americans to live longer, healthier lives and is essential to the viability and prosperity of communities across the country. However, many Americans do not recognize the value that public health systems bring to their communities until these systems are most needed.
Public Health Forward: Modernizing the US Public Health System defines a vision for health in the 21st century and provides a practical, prioritized, bipartisan set of actions for policymakers and public health officials to guide strategic investments and decision-making to achieve this vision. These actions are informed by evidence, build on previous consensus frameworks and objectives, and represent work by national thought leaders that has the support of public health practitioners across the country. The nation’s safety, security, and economic prosperity depends on a strong public health system. We respectfully urge state and local policymakers to act now to fully realize the potential of this unique moment and secure the future of the public’s health.
In 2026, the United States is becoming a healthier nation because elected and public health officials seized the historic opportunity to invest in new and transformative ways to modernize the governmental public health system. The system is prepared to respond to a range of public health challenges, including a pandemic, obesity, mental illness, substance abuse, and climate change. Read the report here.
Stakeholder Engagement Workshop on the Implementation of the United States Government Policy for Institutional Oversight of Life Sciences Dual Use Research of Concern: Workshop Report
A new report documents the discussions of the 2017 Stakeholder Engagement Workshop on the Implementation of the United States Government Policy for Institutional Oversight of Life Sciences Dual Use Research of Concern. It is not an official record of the Stakeholder Engagement Workshop. It was compiled to assist the research and policy communities as they consider updating US Government policies on Dual Use Research of Concern (DURC). Neither the National Institutes of Health nor the National Science Advisory Board for Biosecurity (NSABB) produced a report out of the workshop, and it is hoped that this summary of the discussion, based on analysis of the videos of the workshop, will be useful for those interested in the development of the United States Policies on dual use research of concern.
Daniel Greene and Sam Weiss Evans analyzed the workshop, and drew together four themes from the discussions:
- There are many different ways that institutions have composed their Institutional Review Entities (IREs), which are responsible for assessing the DURC potential of research carried out at the institution.
- While there were a wide array of mitigation strategies employed, institutions rarely used redaction or blocked publications, instead focused on tailoring communication of the scientists, emphasizing the value of the research to the public and avoiding being inflammatory or drawing attention to misuse. Institutions also increased safety and security measures after conducting DURC reviews, and modified experiments to reduce the risks they posed.
- While most of the speakers at the workshop said that DURC policies had minimal impact on research productivity, several participants noted examples of research slowdown, and claimed that oversight burdens had disincentivized potential DURC research, with specific examples of researchers stopping their projects once it became apparent that their research might be DURC.
- The question of whether the overall scope of implementation of the policy was sufficient to capture concerning research appeared throughout the conversations as a central and ongoing challenge. At least six participants at the workshop noted examples of research that either had been done or could be done that could merit the label “DURC”, but that did not involve the 15 agents and 7 experiments of concern named in the USG DURC policy.
United Nations Secretary-General’s Mechanism
Shortly before the end of the conflict between Iran and Iraq, the UN General Assembly passed a resolution in 1987 that established the UN Secretary-General’s Mechanism for Investigation of Alleged Use of Chemical and Biological Weapons (UNSGM). This mechanism serves as a verification instrument of the Geneva Protocol for investigating alleged uses of chemical and biological weapons.
In the framework of the UNSGM, two lists are compiled: one with experts and one with laboratories that can be supported by the UN member states. Spiez Laboratory is on one hand nominated as a designated analytical laboratory and on the other hand provides experts for a mission team in benefit of the UNSGM. For their fact-finding mission in Syria, the UN relied on the laboratory network of the Organisation for the Prohibition of Chemical Weapons (OPCW). The OPCW’s designated laboratories – including Spiez Laboratory – are internationally accredited and subjected to stringent quality tests every year. Since the Chemical Weapons Convention entered into force in 1997, these laboratories have validated their analytical procedures and precisely laid down the criteria for reporting the results.
While there are strict quality standards in the field of chemical weapons, there are no corresponding controls in the biological field. In the case of a UN mission investigating the alleged use of biological weapons, lab analyses might therefore more easily be questioned or even rejected. This is why Spiez Laboratory is committed to establishing corresponding quality assurance and reporting requirements for biological laboratories, so that future UN fact-finding missions relating to biological weapons can also be accepted both politically and scientifically without any reservations.
Apart from the establishment of standards in quality control, continuous advancement of analytical methodology is an important pillar. The developed methods are exchanged between laboratories to further international capacity building in detection of agents. Spiez Laboratory supports these efforts with the organization of a workshop series for designated laboratories of the UNSGM.
Spiez CONVERGENCE intends to inform participants about latest advances on chemistry making biology and biology making chemistry, as well as the adoption of such advances by the biotechnology and chemical industries. Participants discuss how such developments may affect production technologies for toxic chemicals, toxins and microorganisms and assess potential implications for chemical and biological arms control. Read the reports here and here.
Israeli Airstrikes in Syria Targeted Chemical Weapons Facilities, Officials Say
In the middle of the night on 8 June, Israeli warplanes conducted a “highly unusual airstrike deep inside Syrian territory.” The strikes killed seven soldiers, including an engineer who worked at a top-secret Syrian military lab. Following standard operating procedure, the Israel Defense Forces declined to comment on the incursion into Syrian airspace. This attack targeted Syrian military facilities, not the usual Iranian targets. The Washington Post reports that “According to current and former intelligence and security officials briefed on the matter, the June 8 strike was part of a campaign to stop what Israeli officials believe was a nascent attempt by Syria to restart its production of deadly nerve agents.” Dr. Gregory Koblentz, Director of the Biodefense Graduate Program, said, “Syria’s procurement of this chemical, even through black-market channels, is not indicative of a nefarious purpose.” Koblentz further described that “Syria has been hiding key components of its chemical weapons program ever since it signed the Chemical Weapons Convention in 2013.” And given the fact that Syria has regained control over most of its territory, “it makes sense that the Assad regime would want to rebuild its chemical-weapons program to serve once again as a strategic deterrent against its longtime adversary, Israel.”
ALL THINGS COVID-19
Building Apollo’s Arsenal: Acquiring COVID-19’s Lessons Learned for Government – Bioeconomy Partnership
A new brief concludes the CSIS Defense-Industrial Initiative Group’s series on enhancing future biosecurity, examining three cross-national case studies and aspects of the US response, to provide lessons learned from the overall project. The case studies include aspects of three government responses to the COVID-19 pandemic: South Korea’s strategy for testing and diagnostics, New Zealand’s strategy for data management, and China’s strategy for laboratory research. The brief then examines aspects of current US government biosecurity preparations and responses, including the flagship Apollo Project. Lessons learned highlight the importance of accessible, effective data management for both biosurveillance and dispatching supplies to outbreak hotspots. The bioeconomy has the potential to act as surge capacity and innovation reservoir—if mechanisms for coordination and production are established ahead of crisis periods to take advantage of this resource. Likewise, biosecurity research and development (R&D) is a peacetime priority to ensure that resources are ready when they are needed: biosecurity-related defense R&D spending remained relatively flat through the first year of the COVID-19 pandemic, demonstrating that many of the technologies that turned the tide of a pandemic were developed over the years and decades before. Read the report here.
Analyzing COVID-19 Outcomes in the Context of the 2019 Global Health Security Index
The Global Health Security (GHS) Index benchmarks countries’ capacities to carry out the functions necessary to prevent, detect and respond to biological threats. The COVID-19 pandemic served as an opportunity to evaluate whether the Index contained the correct array of variables that influence countries’ abilities to respond to these threats; assess additional variables that may influence preparedness; and examine how the impact of preparedness components change during public health crises. Linear regression models were examined to determine the relationship between excess mortality per capita for the first 500 days of countries’ COVID-19 pandemic and internal Index variables, as well as external variables including social cohesion; island status; perceived corruption; elderly population size; previous epidemic experience; stringency of non-pharmaceutical interventions; and social and political polarization. COVID-19 outcomes were significantly associated with sociodemographic, political and governance variables external to the 2019 Index: social cohesion, reduction in social polarization and reduced perceptions of corruption were consistently correlated with reduced excess mortality throughout the pandemic. The association of other variables assessed by the Index, like epidemiological workforce robustness, changed over time. Fixed country features, including geographic connectedness, larger elderly population and lack of prior coronavirus outbreak experience were detrimental to COVID-19 outcomes. Finally, there was evidence that countries that lacked certain capacities were able to develop these over the course of the pandemic. Additional sociodemographic, political and governance variables should be included in future indices to improve their ability to characterize preparedness. Fixed characteristics, while not directly addressable, are useful for establishing countries’ inherent risk profile and can motivate those at greater risk to invest in preparedness. Particular components of preparedness vary in their impact on outcomes over the course of the pandemic, which may inform resource direction during ongoing crises. Future research should seek to further characterize time-dependent impacts as additional COVID-19 outcome data become available. Read the article here.
Global Percentage of Asymptomatic SARS-CoV-2 Infections Among the Tested Population and Individuals with Confirmed COVID-19 Diagnosis: A Systematic Review and Meta-analysis
What is the percentage of asymptomatic individuals with positive test results for SARS-CoV-2 among tested individuals and those with confirmed COVID-19 diagnosis? In a systematic review and meta-analysis, the authors evaluated the percentage of asymptomatic infections among individuals undergoing testing (tested population) and those with confirmed COVID-19 (confirmed population). The review included cross-sectional studies, cohort studies, case series studies, and case series on transmission reporting the number of asymptomatic infections among the tested and confirmed COVID-19 populations that were published in Chinese or English. From the analysis of 95 unique studies with 29,776,306 individuals undergoing testing, the pooled percentage of asymptomatic infections was 0.25% among the tested population and 40.50% among the population with confirmed COVID-19. The high percentage of asymptomatic infections highlights the potential transmission risk of asymptomatic infections in communities. Read the article here.
How COVID Vaccines Shaped 2021 in 8 Powerful Charts
A year ago, vaccine drives against COVID-19 were just beginning. Now, more than 4.4 billion people have had one or more dose — about 56% of the world population. The vaccination of so many in such a short space of time, so soon after the unparalleled rapid development of the vaccines, has saved huge numbers of lives and is a triumph for science and research. Sadly, the vaccines have not been shared or taken up equitably across the world, nor even, sometimes, within nations. But the extraordinary roll-out of a plethora of COVID-19 vaccines — or the lack thereof — has been a major force shaping politics, science and everyday human experience in 2021. In a graphic-led story, available here, Nature offers a guide to the successes, failures and impact of COVID-19 vaccines in 2021.

The Government Asked Us Not to Release Records From The CDC’s First Failed COVID Test. Here They Are.
In February 2020, nine officials at the Centers for Disease Control and Prevention (CDC) convened with an expert from the Food and Drug Administration (FDA) to figure out why the nation’s first coronavirus test failed. The CDC had already sent out thousands of flawed test kits to nearly 50 public health labs across the country. It turned out the reagents of the tests were likely contaminated at the small, underfunded Respiratory Virus Diagnostic (RVD) Lab. A short report from the Department of Health and Human Services (HHS) was released in June 2020 and it summarizes that “the findings of the Office of the General Counsel (OGC) regarding the Centers for Disease Control and Prevention (CDC) manufacturing of the initial COVID-19 test kits that could not be validated by public health laboratories.” An email sent from a lab official to CDC leadership three days after the report was released “called into question the central conclusion that the respiratory virus lab was to blame.” This email stated that “the report contained false statements and that HHS investigators had received genetic test results showing that the real source of the contamination was the core lab positive controls — revealed by their distinct genetic signature.” Another email stated that the contamination in the COVID test kits did “not match the cloned coronavirus gene made by the RVD lab to serve as positive controls.” To date, the CDC has not released an official explanation of the problem, nor has the HHS inspector general released their report.
We Have Enough COVID Vaccines for Most of the World. But Rich Countries Are Stockpiling More Than They Need for Boosters.
It has now been two years since SARS-CoV-2 first emerged in humans, and pharmaceutical companies have pushed out “enough vaccines to inoculate most of the world against COVID-19.” Yet, dozens of developing nations are struggling with dire shortages as rich countries develop their stockpiles with “hundreds of millions more doses than they need.” According to Duke’s Global Health Innovation Center and the COVID Collaborative, there are about 11 billion COVID-19 vaccine doses will have been manufactured by the end of 2021. STAT emphasizes that “overall, 56% of the global population has received at least one dose, but those vaccines are wildly unevenly distributed, with just 7.1% of people in low-income countries having received at least one dose.” About 847 million more doses are needed to bring all countries up to the 40% vaccination rate. Analyses show, shockingly, that the “vaccine shortage for low-income countries is less than the surplus vaccines within the G7 countries and the European Union.” According to STAT, “vaccines could be distributed internationally faster if wealthier countries allowed COVAX or countries in dire need to take newly created vaccines first; just Switzerland and the US have done so.” The Access to COVID-19 Tools (ACT) Accelerator, which brings together governments and global health organizations including the WHO and Gavi, the Vaccine Alliance, recently announced an additional $23.4 billion is needed for vaccine distribution by September 2022.
Playing With Fire: Terrifying COVID Lab Leak Feared to Have Infected Dozens in Taiwan in Chilling Echo of Wuhan
A female laboratory worker in Taipei tested positive for coronavirus and may have caught it from working on experiments in a Biosafety Level-3 lab. Authorities have started tracing over 85 people as contacts of the infected worker. This incident follows research by Dr. Filippa Lentzos and Dr. Gregory D. Koblentz regarding high containment labs across the world. Their work highlights the significant risks created by these labs amid the pandemic. More specifically, BSL-4 labs are designed to work with dangerous viruses for which there are no vaccine or treatments. Lentzos and Koblentz emphasize that the “risks of work with dangerous pathogens mean that extremely high-levels of safety and security protection must be applied and that the work must be conducted responsibly.”
Pandora Report: 12.10.2021
Dr. Gregory Koblentz, Director of the Biodefense Graduate Program, poignantly emphasized, “when great powers compete during a pandemic, the only winner is the virus.” The 2021 GHS Index measures the capacities of 195 countries to prepare for epidemics and pandemics, and found that all countries remain dangerously unprepared for future epidemic and pandemic threats. State medical boards are receiving more and more complaints about false or misleading information about COVID-19, but only a handful have “taken action against doctors.”
Biodefense Vision of the Defense Secretary
A recent memorandum introduces Secretary of Defense’s Vision for Biodefense:
Since taking office, President Biden has emphasized the importance of bold approaches to defeat the current coronavirus disease 2019 (COVID-19) pandemic, as well as transform the Nation’s approach to biodefense. We must prepare to operate in a biological threat environment and support the National biodefense enterprise, both at home and abroad. To support that vision, the Department of Defense (DoD) will prioritize biodefense across the full spectrum of biological threats, from naturally occurring to accidental and deliberate biological incidents.
During the COVID-19 pandemic, the Department’ s preparation and response enabled it to protect DoD personnel, safeguard the DoD mission, and support a whole-of-nation response. However, after-action reviews have identified areas for improvement across the DoD biodefense enterprise that must be addressed. Therefore, I direct the Department to continue to fortify our immediate pandemic preparedness and to undertake a comprehensive Biodefense Posture Review (BPR). This review will assess the biological threat landscape and establish the Department’ s approach to biodefense, to include clarifying biodefense priorities, roles, responsibilities, authorities, capabilities, and posture.
Three principles will guide the Department’ s posture review: 1) Unify efforts through an empowered, collaborative, and integrated approach to biodefense across the Department; 2) Modernize DoD operations to optimize capabilities, capacity, resilience, and readiness; and 3) Synchronize biodefense planning with the Department’s new National Defense Strategy and with the efforts of other Federal departments and agencies and, as appropriate, allies and partners, to support national biodefense efforts in alignment with national goals and strategy.
The Deputy Secretary of Defense will oversee this work and provide implementation guidance for the BPR and pandemic preparedness efforts. The Under Secretary of Defense for Policy and Under Secretary of Defense for Acquisition and Sustainment will co-lead the BPR. Every component across DoD plays a role in biodefense; I expect that the entire Department will play a constructive role in this review.
2021 Global Health Security Index
The 2021 GHS Index measures the capacities of 195 countries to prepare for epidemics and pandemics. All countries remain dangerously unprepared for future epidemic and pandemic threats, including threats potentially more devastating than COVID-19. The Index found that although many countries were able to quickly develop capacities to address COVID-19, all countries remain dangerously unprepared for meeting future epidemic and pandemic threats. A great opportunity exists, however, to make new capacities more durable to further long-term gains in preparedness. Countries should allocate health security funds in national budgets and conduct assessments using the 2021 GHS Index to develop a national plan to identify their risks and fill gaps. International organizations should use the GHS Index to identify countries most in need of additional support. The private sector should use the GHS Index to look for opportunities to partner with governments. Philanthropies and funders should develop new financing mechanisms and use the GHS Index to prioritize resources. Read the report’s findings and recommendations, explore the data, view the country rankings, and learn more about the GHS Index.
Briefing by Mr. Christian Ritscher Special Adviser and Head of the United Nations Investigative Team to Promote Accountability for Crimes Committed by Da’esh / Islamic State in Iraq and the Levant
Christian Ritscher, Special Adviser and Head of the United Nations Investigative Team to Promote Accountability for Crimes Committed by Da’esh/Islamic State in Iraq and the Levant, gave a statement earlier this month.
“A week ago, I stood at a mass grave outside Mosul containing the remains of the victims of executions carried out by ISIL at Badush Central Prison in June 2014. I listened to the story told by one survivor who had to go through this horror, and now has to carry its magnitude as he seeks to move on with his life. I also saw the commitment demonstrated by the national authorities and our team members as well as other partners, working in this remote location, despite the security challenges, to support the collection of evidence that may lay the foundations for justice, and to ensure that families will be able to bury the remains of their loved ones.
Evidence collected shows the detailed preparation of the attack by senior ISIL members, followed by the launch of the assault on the morning of 10 June. Prisoners captured were led to sites close to the Prison, separated based on their religion and humiliated. At least one thousand predominantly Shia prisoners were then systematically killed.
Through our analysis of digital, documentary, testimonial and forensic evidence, including internal ISIL documents, we have identified a number of individual ISIL members responsible for carrying out these crimes. Through the synthesis of this data, I can also announce to the Council today that we have finalized our initial case-brief in relation to this investigation, detailing our conclusion that crimes committed by ISIL members at Badush Central Prison constitute crimes against humanity of murder, extermination, torture, enforced disappearances, persecution and other inhumane acts, and the war crimes of wilful killing, torture, inhumane treatment, and outrage upon personal dignity.
By establishing this comprehensive structural analysis of crimes committed at Badush prison, as we have previously with respect to attacks in Sinjar and Tikrit, we seek to strengthen the basis on which justice can be built together with national authorities.
We now have the chance, collectively, to make such prosecutions the norm, not a celebrated exception. In cooperation with Iraqi authorities and those of the Kurdistan region, together with survivors and with the support of this Council, we are building the evidence that can deliver meaningful justice for all those who suffered from ISIL crimes in Iraq. If we maintain our unity, we can capitalize on the opportunity that is now before us.”
Read the full briefing here.
Creating Dangerous Viruses in the Lab Is a Bad Way to Guard Against Future Pandemics
Dr. Lauren Kahn, a physician and policy researcher, discussed the risks associated with studying dangerous viruses. In 2011, an opinion piece was written by three top US government scientists on why research invoking the modification of highly pathogenic avian influenza (H5N1) was a worthy undertaking. Concurrently, the National Institutes of Health (NIH) was experiencing “blowback from funded experiments that modified the virus to be transmissible among ferrets.” Amid this controversy, the US government put a pause on 2014 federal funding for “selected research reasonably anticipated to increase transmissibility or pathogenicity of influenza, SARS, and MERS viruses.” Such research fell into the category of gain-of-function work. Kahn highlighted that “the federal government continues to fund such experimentation, but, as scientists, media, and online sleuths have delved into the origins of COVID-19, they have revealed weaknesses in past and current government oversight of projects modifying viruses.” But federal funding now supports this type of experimentation, especially as we battle the novel coronavirus. In regard to the pandemic, Kahn states that “ideally, Congress should hold a hearing to debate what kind of research should not be done and do more to investigate the origins of the pandemic.” In summary, “preventing pandemics through rapid identification and response is an important goal; the One Health approach that emphasizes animal and human health and disease surveillance is the key to doing this, not risky gain-of-function research.”
The Hot Zone, Season 2
National Geographic’s The Hot Zone: Anthrax follows the team of experts tracking down the killer and mailer of the anthrax letters. The six episodes in this season feature Tony Goldwyn as microbiologist Bruce Ivins, the suspected perpetrator of the actual 2001 anthrax attacks. Daniel Dae Kim stars as Matthew Ryker, an FBI agent specializing in microbiology. The trailer is available here.
Spring 2022 Open Courses: BIOD 762 & 766
For any GMU graduate students, the Biodefense Program is offering a couple fascinating courses this coming spring semester! Biotechnology and Society (BIOD 762) examines the growing role of biotechnology in modern society, including benefits to human and animal health, industrial applications, and potential for misuse. This course will be taught by Dr. Lauren Quattrochi, a classically trained as an electrophysiologist and neuro-pharmacologist. Development of Vaccines and Therapeutics (BIOD 766) is possibly more relevant now than ever before! The course analyzes the process of developing new medical countermeasures against biological weapons and emerging infectious diseases such as SARS and pandemic influenza, and gives special attention to the scientific, technical, political, regulatory, and economic obstacles to developing new vaccines and therapeutics. Dr. Robert House, who has a PhD in medical parasitology and is Senior Vice President of Government Contracts at Ology Bioservices, will be teaching BIOD 766.
ALL THINGS COVID-19
Jabbed in the Back: Mapping Russian and Chinese Information Operations During COVID-19
The Center for European Policy Analysis (CEPA) released a report, Jabbed in the Back, as part of a broader CEPA research project aimed at tracking and evaluating Russian and Chinese information operations around COVID-19.
During the COVID-19 pandemic, the Chinese Communist Party (CCP) spread disinformation about the efficacy of vaccines and the virus’s origins, a shift from Beijing’s previous disinformation campaigns, which had a narrower focus on China-specific issues such as Tibet, Hong Kong, and Taiwan. Most of Beijing’s COVID-19 narratives aimed at shaping perceptions of China’s response to the pandemic and only rarely targeted other countries specifically. Russia recycled previous narratives and exacerbated tensions in Western society while attempting some propaganda about Russian scientific prowess. The Kremlin and the CCP learned from each other. While limited evidence exists of explicit cooperation, instances of narrative overlap and circular amplification of disinformation show that China is following a Russian playbook with Chinese characteristics. Russia is simultaneously learning from the Chinese approach. The largest difference between China’s and Russia’s information warfare tactics remains China’s insistence on narrative consistency, compared with Russia’s firehose of falsehoods strategy. Even with substantially greater resources, this largely prevents Chinese narratives from swaying public opinion or polarizing societies. The two authoritarian countries’ information operations have evolved over the last 18 months and will continue to do so with the spread of variants, vaccines, and inquiries into the virus’s origins. Read the report here.
Some Doctors Spreading Coronavirus Misinformation Are Being Punished
State medical boards are receiving more and more complaints about false or misleading information about COVID-19, but only a handful have “taken action against doctors.” The Federation of State Medical Boards surveyed its 70 member boards across the nation this fall, and found two concerning statistics. More than two-thirds of the 58 responding boards saw an “uptick” in complaints, and only a dozen boards “reported taking some sort of disciplinary action against doctors for spreading false or misleading information.” Rachel Moran, a researcher at the University of Washington who studies coronavirus misinformation, said that misinformation delivered by doctors can be “particularly insidious” as a result of the credibility associated with their profession and the difficulty that patients may experience try to “debunk” their highly technical language. The Federation of State Medical Boards issued a statement in July “warning that doctors who spread coronavirus vaccine misinformation risk disciplinary action, including the revocation of their license.” The Federation stated that physicians bear an “ethical and professional responsibility to practice medicine in the best interests of their patients,” and this obligation is violated when they spread inaccurate information. Other certifying boards soon followed their statement, such as the American Board of Family Medicine, American Board of Internal Medicine and American Board of Pediatrics. At present, a handful of medical doctors have lost their licenses. For example, the Oregon Medical Board pulled the license of a doctor “who refused to follow public health guidelines in his clinic, spread misinformation about masks and overprescribed opioids.” On the flip side, some doctors have maintained or renewed their licenses “despite making dangerous statements about the virus.” For instance, Ohio-based licensed osteopathic physician and anti-vaccine advocate Sherri Tenpenny claimed that the COVID-19 vaccines could leave people “magnetized” and North Carolina osteopathic physician Rashid Buttar who has falsely stated that the COVID-19 vaccines “kill more people than COVID-19.”
The Uneven COVID-19 Vaccine Rollout
US President Biden has set a goal for 70% of the world’s population to be vaccinated against COVID-19 by the end of 2022. Currently, 45% of the world’s population has received the full number of doses prescribed by the vaccination protocol, according to Our World in Data.
After what has now been a year since the first person outside of clinical trials received a COVID vaccine, the global rollout is still a long way from reaching this target. As the following infographic shows, it has also been uneven. The highest proportion of the population fully vaccinated is in South America, at 60%. Europe is close behind with 59%. Oceania, North America and Asia line up close behind, all above 50% as 2021 comes to a close. In Africa though, a mere 8% have been fully vaccinated.
In summary: “We must do better.”

Advancing US-China Health Security Cooperation in an Era of Strategic Competition
Although the United States and China have entered a period of strategic competition, bilateral cooperation on health security is more important than ever. The COVID-19 pandemic, with its novel nature and devastating impact globally, represents another critical opportunity for bilateral cooperation. A high-profile strategy to promote cooperation may achieve minimal traction when facing barriers that are difficult to overcome. One must remain realistic about what can be achieved in the near term. A new report from the Center for Strategic and International Studies (CSIS) report lays out six concrete, actionable streams where there could be collaborative work. Three areas of cooperation—travel, public health infrastructure, and supply chain resilience—stand out as most likely to deliver substantive results in the short term. They face relatively few barriers to implementation but could generate major positive spillover effects. US-China health cooperation in another three areas—vaccines and therapeutics, biosafety and biosecurity, and countering disinformation—also promises high benefits for improving health security but faces higher substantive and political hurdles. The proposals suggested here can be advanced through a mixed, forward-looking strategy that involves mobilizing multiple stakeholders in promoting US-China cooperation over health security, including intervention from top leaders from both sides. There are political, economic, and practical obstacles at almost every turn, and the United States should proceed with appropriate caution and care. But the opportunity space for engaging China remains larger than the risks of not doing so. At the same time, strengthening America’s health security is critical to the national interest and needs to be understood as an urgent challenge. Time is of the essence. As, Dr. Gregory Koblentz, Director of the Biodefense Graduate Program, poignantly emphasized, “when great powers compete during a pandemic, the only winner is the virus.” Read the report here.
OMICRON
President Biden Announces New Actions to Protect Americans Against the Delta and Omicron Variants as We Battle COVID-19 this Winter
President Biden announced new actions to combat COVID-19 as the United States heads into the winter months and with the emergence of a new variant, Omicron. The United States has come far in its fight against the virus and is more prepared than ever to deal with the challenges of COVID-19. We have the public health tools we need to continue to fight this virus without shutting down our schools and businesses. As we head into winter, the President announced actions to provide additional protection to Americans and fight the Omicron and Delta variants, while keeping our economy growing. This plan includes:
- Boosters for All Adults
- Vaccinations to Protect Our Kids and Keep Our Schools Open
- Expanding Free At-Home Testing for Americans
- Stronger Public Health Protocols for Safe International Travel
- Protections in Workplaces to Keep Our Economy Open
- Rapid Response Teams to Help Battle Rising Cases
- Supplying Treatment Pills to Help Prevent Hospitalizations and Death
- Continued Commitment to Global Vaccination Efforts
- Steps to Ensure We Are Prepared for All Scenarios
Implications of the Mutations in the Spike Protein of the Omicron Variant of Concern (VoC) of SARS-CoV-2
Dr. Gene Godbold, Senior Scientist at Signature Science, provided a summary of the science related to the Omicron variant of concern of SARS-CoV-2. The omicron variant appears to have arisen in Africa, perhaps Botswana, and was first detected by the viral sequencing efforts of neighboring South Africa in November of 2021. The changes in Spike protein, relative to other variants, have concerned virologists and public health personnel. The Spike of omicron has 30 amino acid changes, one insertion of three amino acids and three small deletions when compared to the original Wuhan strain. The net effect of the insertions and deletions is the loss of three amino acids relative to the Wuhan strain.
Spike is the best studied of all the proteins produced by the SARS-CoV-2 virus. It largely, but not solely, governs the host immune response to the virus. Spike is responsible for both the adherence of the virus to host cells and the invasion of the virus into cells. Those two features are critical for viral transmission. All the vaccines that are currently available worldwide target Spike.
The mutations in the Spike protein of the omicron variant of SARS-CoV-2 are likely to result in a more transmissible variant and one that can evade neutralizing antibodies induced by vaccination better than previously seen variants. This is not to suggest that vaccination is likely to be defeated by the omicron variant, only that the protection conferred by vaccination is likely to be shakier than with previous variants of concern. The activated immune system is a potent defender, however, with many weapons to fight infection that are not altogether dependent upon the antibody response. Read the full explanation here.
EVENTS
ICYMI: COVID-19 and Intelligence
The COVID-19 pandemic has wreaked havoc on everything from global supply chains to individual lives, with its long-term implications only beginning to take shape. Pandemics, a public health issue, are proving to be a national security one as well. Are America’s national security institutions prepared to address this threat? What role should the intelligence community play? What reforms could improve global health surveillance?
he Michael V. Hayden Center for Intelligence, Policy, and International Security and the Schar School’s biodefense program presented a discussion on these questions. Panelists includes Rep. Eric Swalwell (CA-15), a four-term congressman at the forefront of legislative efforts to reform the intelligence community’s approach to pandemic awareness; Dr. Julie Gerberding, who served as director of the Centers for Disease Control and Prevention from 2002 to 2009, where she led the agency through the SARS outbreak, and is currently a senior leader at the pharmaceutical company Merck; and Matt Berrett, a former CIA assistant director and head of its Global Issues Mission Center, and cofounder of the Center for Anticipatory Intelligence at Utah State University. David Priess, our senior fellow and publisher and chief operating officer of Lawfare, moderated the event.
The panel was recorded and is available here. A related episode of Priess’ Lawfare Podcast is available here.
Building Apollo’s Arsenal: Acquiring COVID-19’s Lessons Learned for Government-Bioeconomy Partnership
Please join the CSIS Defense-Industrial Initiatives Group for a conversation on enhancing the future of biosecurity. The discussion will celebrate the launch of our new brief, which examines the ways that diagnostics, data, research and development undergird biosecurity preparedness and response. The panel will center on what comes next: what can policymakers do now to ensure the future of biosecurity remains strong? What government acquisition mechanisms can draw on the innovation of the bioeconomy? The ambitious Apollo Program for Biodefense demonstrates the current moment’s momentum, but what programs will be resilient, even after COVID-19 fades from the headlines? This webinar is scheduled for 14 December at 1:30 PM EST. Register here.
US-China Health Security Cooperation: Time is of the Essence
Although the United States and China have entered a period of strategic competition, bilateral cooperation on health security is of paramount importance. A new report from the CSIS Commission on Strengthening America’s Health Security – authored by Yanzhong Huang, Senior Fellow for Global Health at the Council on Foreign Relations, and Scott Kennedy, CSIS Senior Adviser and Trustee Chair in Chinese Business and Economics – lays out six concrete, actionable streams for collaboration.
Please join the CSIS Trustee Chair in Chinese Business and Economics and CSIS Commission on Strengthening America’s Health Security for a discussion on the key takeaways of the report. Panelists will include Xiaoqing Boynton, Senior Director of International Affairs at the Biotechnology Innovation Organization; Tom Frieden, President and CEO of Resolve to Save Lives; Deborah Seligsohn, Senior Associate with the CSIS Trustee Chair in Chinese Business and Economics and Assistant Professor of Political Science at Villanova University. Scott Kennedy will provide a background of the report and Yanzhong Huang will provide a summary of the report’s policy recommendations, respectively. J. Stephen Morrison, Senior Vice President and Director of the CSIS Global Health Policy Center, will host and moderate the discussion. This live webcast will be held 14 December at Noon EST. Register here.
Pandora Report: 12.3.2010
For Biodefense graduate students looking for a fascinating course to round out your spring semester, Dr. Robert House is offering a course on the development of vaccines and therapeutics, and Dr. Quattrochi is teaching a course on biotechnology and society! The Bioeconomy Information Sharing and Analysis Center, or BIO-ISAC, released an advisory regarding an advanced persistent threat (APT) attack named Tardigrade. The World Health Assembly agreed to kickstart a global process to draft and negotiate a convention, agreement or other international instrument under the Constitution of the World Health Organization to strengthen pandemic prevention, preparedness and response.
Spring 2022 Open Courses: BIOD 762 & 766
For any GMU graduate students, the Biodefense Program is offering a couple fascinating courses this coming spring semester! Biotechnology and Society (BIOD 762) examines the growing role of biotechnology in modern society, including benefits to human and animal health, industrial applications, and potential for misuse. This course will be taught by Dr. Lauren Quattrochi, a classically trained as an electrophysiologist and neuro-pharmacologist. Development of Vaccines and Therapeutics (BIOD 766) is possibly more relevant now than ever before! The course analyzes the process of developing new medical countermeasures against biological weapons and emerging infectious diseases such as SARS and pandemic influenza, and gives special attention to the scientific, technical, political, regulatory, and economic obstacles to developing new vaccines and therapeutics. Dr. Robert House, who has a PhD in medical parasitology and is Senior Vice President of Government Contracts at Ology Bioservices, will be teaching BIOD 766.
Agricultural Production, Traditional Foods and Household Food Insecurity in Rural Kenya: Practice, Perception and Predictors
Although rural households in Kenya rely on agricultural production for their livelihood, attaining food security is challenging in areas experiencing harsh agro-ecological conditions. We utilized mixed methods research to examine the effect of agricultural production, including that of traditional foods, on household food insecurity in Seme sub-County of Kenya. Study participants believed that traditional foods protected against hunger. However, production of these foods, with the exception of traditional vegetables, was low. Poultry-keeping; cereal/grain, any vegetable and traditional vegetable production; and crop diversity were significantly associated with lower household food insecurity. Vegetable production maintained statistical significance after controlling for other variables. Professor Bonnie Stabile, Associate Professor and Associate Dean of Student and Academic Affairs in the Schar School, was a co-author of this publication. Phil Thomas is an adjunct professor for the Biodefense Graduate Program who teaches the Threats to Global Food Security course. Read the article here.
You Should Be Afraid of the Next ‘Lab Leak’
In Boston stands a seven-story fortress that houses the National Emerging Infectious Diseases Laboratories (NEIDL), and it contains a large collection of Biosafety Level 4 and Biosafety Level 3 labs. These high-containment labs conduct research on some of the deadliest pathogens, like Lassa and Marburg viruses. An accident that resulted in one of these lethal microbes escaping could spur another outbreak and even another pandemic. Six years ago, the National Institutes for Health commission Gryphon Scientific, a consulting firm, to conduct a risk assessment of certain types of research at US facilities. The assessment led to a thousand-page report, which found that “that experiments to improve the transmissibility of coronaviruses in a lab could significantly increase the chance of a pandemic due to a laboratory accident.” It also noted that “loss of containment” incidents for viruses are rare, and that a breach would “not necessarily mean an outbreak.” Even an escaped pathogen with pandemic potential “would have a low chance of leading to a global crisis.”
Dr. Filippa Lentzos and Dr. Gregory Koblentz conducted a study of Biosafety Level 4 labs around the world and calculated that there are 59 in operation, under construction, or in the planning stages. Lentzos stated that “these labs are there so we can work with these pathogens in safe, secure ways,” but “these labs are spreading into other parts of the world, where you have different kinds of regimes, more authoritarian regimes, for instance, where the concept of openness is particularly challenging.”
Public & Private Funding Opportunities to Advance a Circular US Bioeconomy and Maintain US Biotechnology Competitiveness
In the nearly 50 years since the first genetic engineering experiments, the United States has become the world’s biotechnology powerhouse, with the resulting biology-based economy—the bioeconomy—generating nearly $960 billion in economic activity in 2016, about 5 percent of US GDP, with more than half of the total generated outside the biomedical sector, including the agricultural and industrial biotechnology sectors. Over the next two decades or less, a well-developed bioeconomy has the potential to transform manufacturing processes to use renewable biomass rather than petroleum to make the products of modern society, and in doing so, reduce the nation’s dependence on fossil fuels, revitalize US manufacturing and employment across the nation, create a more resilient supply chain, improve the nation’s health, and contribute significantly to the goal of creating a net zero greenhouse gas economy. However, decentralized leadership, inadequate talent development, insufficient investment in both fundamental research and developing bioprocessing infrastructure, and international competition put the United States at risk of forfeiting that world-leading position and squandering the entrepreneurial drive and capital market interest that is trying to expand the bioeconomy. Without concrete action to address these concerns, the nation’s economy, its national security, the health of its residents, and its opportunity to move to a net zero economy that creates good-paying jobs and keeps them in the country are in peril.
Schmidt Futures, a philanthropic initiative of Eric and Wendy Schmidt, convened a Task Force to chart a course for achieving the promise of platform technologies such as synthetic biology and artificial intelligence to contribute to what has recently been projected to become a future $4 trillion global bioeconomy. The Task Force deliberated the roadblocks and focused on identifying opportunities for translating basic science research into products for the general public by enabling large scale production of exciting bioeconomy products that are ready to move out of the lab, such as:
- a new generation of plastics that degrade to harmless chemicals in seawater and soil
- biologically produced, carbon-neutral cement
- alternative food protein sources that use less water and land and produce fewer greenhouse gas emissions
- climate change resilient plants, including salt- and drought-resistant crops
- textiles and dyes whose production slashes carbon dioxide emissions and reduces toxic waste
- soil microbes that reduce fertilizer use, improve the health of soils, and remove carbon dioxide from the atmosphere
This report from makes recommendations for public and private action that fall into two broad categories: foundational science and technology challenges and scale-up capacity bioproduction infrastructure. Read the report here.
Results of a 2020 Survey on Reporting Requirements and Practices for Biocontainment Laboratory Accidents
Biosafety laboratory accidents are a normal part of laboratory science, but the frequency of such accidents is unclear due to current reporting standards and processes. To better understand accident reporting, a survey was created, with input from ABSA International, which included a series of questions about standards, requirements, and likely motivations for reporting or nonreporting. A total of 60 biosafety officers completed the survey. Respondents reported working with more than 5,000 people in laboratories, including more than 40 biosafety level 3 or animal biosafety level 3 laboratories, which work with higher-risk pathogens. Most of the respondents were located in the United States, Canada, or New Zealand, or did not identify their location. Notable results included that 97% of surveyed biosafety officers oversee laboratories that require reporting exposure to at least some pathogens. However, 63% relayed that the reports are not usually sent outside of the institution where they occurred. A slight majority (55%) stated that paper reports were used, with the rest reporting they used a variety of computer systems. Even in laboratories that used paper-based reporting systems, 67% relayed that these reports were used alongside, or entered into, a digital system. While 82% of these biosafety officers agreed that workers understood the importance of reporting for their own safety, 82% also agreed that a variety of disincentives prevent laboratory workers from reporting incidents, including concerns about job loss and loss of funding. Read the article here.
As Supply Lines Strain, Some Corporations Rewrite Production Playbook
The COVID-19 pandemic interrupted a number of supply chains across the globe. Now, 23 months in, companies are still struggling to strengthen their supply chains. For example, Stanley Black & Decker has accelerated plans to open two new factories, one in Mexico and one in Texas. The company has also “locked in future supplies of lithium-ion batteries for power tools by funding dedicated production capacity at US and Taiwanese suppliers and stockpiled an extra $1 billion in products.” Don Allan, the chief financial officer of Stanley Black & Decker, said, “the more you can minimize the amount of time your product is in transit, the better off you’re going to be.” Companies are employing an array of tactics to solve their supply chain problems, at least temporarily. Colgate Palmolive used more expensive airfreight to ship its toothpaste and toothbrushes, and Walmart chartered its own ships. For longer term solutions, companies are “moving production to new suppliers or different countries and relaxing their traditional fixation with low costs.” Some goods are finalized at factories with components arriving “just in time” as freight costs skyrocket and delivery times fluctuate.
BIO-ISAC Releases Advisory to Biomanufacturers – Tardigrade: An APT attack on vaccine manufacturing infrastructure
The Bioeconomy Information Sharing and Analysis Center, or BIO-ISAC, released an advisory regarding an advanced persistent threat (APT) attack named Tardigrade. A large biomanufacturing facility was involved in a cyberattack in Spring 2021. Through the subsequent investigation, a malware loader was identified that demonstrated a high degree of autonomy as well as metamorphic capabilities. In October 2021, further presence of this malware was noted at a second facility. Due to the advanced characteristics and continued spread of this active threat, BIO-ISAC made the decision to expedite this threat advisory in the public interest. Analysis continues, and updates will be released on isac.bio as further details are made available. At this time, biomanufacturing sites and their partners are encouraged to assume that they are targets and take necessary steps to review their cybersecurity and response postures.
Biosecurity Diplomacy Workshop for Young Scientists from the Global South
The United Nations Office for Disarmament Affairs (UNODA) Geneva Branch and the Implementation Support Unit (ISU) of the Biological Weapons Convention (BWC) are delighted to open the call for applications for the third edition of Biosecurity Diplomacy Workshop for Young Scientists from the Global South. The workshop is taking place in the framework of European Union Council Decision 2019/97/CFSP in support of the BWC.
The global norm against biological weapons cannot be maintained without youth voices being included in the multilateral discussions taking place in the framework of the BWC. As fast-paced innovation in biotechnologies raises global implications for biosecurity, the young scientists of today will be on the forefront of tomorrow’s collective and innovative global solutions. This vision was stated explicitly in the UN Secretary-General’s Disarmament Agenda “Securing Our Common Future”, in which youth participation is recognized as a pre-condition to achieve the Sustainable Development Goals.
The workshop is an interactive training programme aiming at informing young scientists about their critical role in biosafety and biosecurity and bolstering global capacities against the misuse of biological agents. It will allow a new cohort of up to 30 future-oriented young biosecurity specialists from the Global South to reflect on how they envision an innovative and bio-secure future in connection with the BWC.
The workshop is open to those who: are under the age of 40; are citizens of a low- or middle-income BWC State Party; have an advanced degree in the life sciences or a related discipline from a recognized university or institution; have backgrounds in other fields such as social sciences, but have a demonstrated interest in biosecurity and/or disarmament and non-proliferation; and have a strong command of written and spoken English, as the workshop will be fully conducted in English. The deadline to receive applications is 6 December 2021, midnight CET.
BWC
BWC: Report of the Meeting of States Parties
The Meeting of States Parties to the Convention on the Prohibition of the Development, Production and Stockpiling of Bacteriological (Biological) and Toxin Weapons and on Their Destruction was pushed to last year as a result of the COVID-19 pandemic. The Meeting was held in Geneva from 22 to 25 November 2021. An advance version of the Report of the Meeting of States Parties is available here.
Remarks to the 2021 Biological Weapons Convention Meeting of States Parties
Ambassador Bonne Denise Jenkins, Under Secretary for Arms Control and International Security, gave her remarks to the 2021 Biological Weapons Convention Meeting of State Parties. An excerpt of her statement is below:
“For the past two decades, efforts to strengthen the Convention have been treading water. Useful discussions here have led to some small steps and actions at the national level. However, States Parties have been unable to agree to more significant action. We face a biological weapons threat that is real, serious, and, in many respects, growing. Some states continue to possess sophisticated, well-established biological weapons programs, while non-state actors have shown continuing interest in acquiring BW capabilities. Additionally, widespread availability of sophisticated scientific and technological tools and methods is gradually eroding barriers to the development of biological weapons.
While COVID-19 was not the result of a biological weapon, the pandemic is a wake-up call for all of us. The astonishing human toll of the pandemic has illustrated our shared vulnerability to novel pathogens. Unprecedented efforts are now underway to strengthen international health security, but we need to address not only the latest challenge, but those that may lie ahead, whether natural, accidental, or deliberate in origin. To do so, we must strengthen the BWC, as National Security Adviser Jake Sullivan said in his November 19 statement. The status quo is neither acceptable nor up to the task. We must take action to ensure that the Convention can effectively address the challenges we face now and in the future. We cannot keep treading water.
The first step is to overcome the political impasse of the last twenty years. We envision a two-pronged approach. The Review Conference should take near-term, concrete action to strengthen the Convention and benefit States Parties. These actions include further operationalizing assistance under Article VII; establishing a voluntary fund for technical cooperation; creating a mechanism to review advances in science and technology; deepening collaborations on biosafety and biosecurity; staffing the Implementation Support Unit to carry out these roles; and enabling more agile decision making. The second way forward is for Review Conference to also take steps to address the harder issues. It should establish a new expert working group to examine possible measures to strengthen implementation of the Convention, increase transparency, and enhance assurance of compliance. Such an effort should consider both advancements in science and technology as well as changes in the nature of the threat. As we are all acutely aware, a great deal has happened in the last two decades. It could be useful to build on some approaches suggested in past discussions, but our efforts should not be defined by them.”
Read her full statement here.
Statement to the Biological Weapons Convention Meeting of States Parties United Nations Geneva, 22 November 2021
At the Meeting of State Parties in Geneva, Switzerland, Dr. Gregory Koblentz, Director of the Biodefense Graduate Program, presented remarks drafted by himself and Dr. Filippa Lentzos from the Department of War Studies and Centre for Science & Security Studies at King’s College London. Following is an excerpt from the statement:
“One of the most politicised aspects of COVID-19 has been the question of how the pandemic started. One theory is that the virus spilled over naturally from animals to humans. Another theory is that it originated from scientific research where the virus accidentally escaped from a laboratory or scientists were infecting during fieldwork when they were collecting viral samples from bats.
It is likely we will never know the answer with any real level of confidence. We are now nearly two years into the pandemic and we’ve still not had a credible international investigation. Unfortunately, there are no signs that we will get one any time soon either. But what we do know is that it is possible to produce biological weapons that are worse than COVID-19. And we do know that dangerous viruses can escape from many labs around the world.
Dangerous viruses have been created in labs during the course of regular scientific research for many years now.
Only a handful of countries with BSL4 labs have oversight or regulatory policies in place for dual-use research. This means that the vast majority of countries with BSL-4 labs do not have specific oversight of high-risk gain-of-function research that has been a central feature in the debate on COVID-19’s origin.
We emphatically support the joint NGO statement’s call for consistent implementation of international standards on appropriate biorisk management practices, especially in laboratories working with high-risk zoonotic pathogens with pandemic potential.”
Read the full statement here.
Statement by National Security Advisor Jake Sullivan on the US Approach to Strengthening the Biological Weapons Convention
COVID-19 was a wake-up call for humanity. It revealed the devastating impact of infectious disease on our health and our societies. It also uncovered our shared vulnerability to catastrophic biological events and the lost lives, economic downturn, and global destabilization that they can cause. As we work to end the COVID-19 pandemic, we must simultaneously recognize that biological risks are growing. We face an increased threat of naturally occurring emerging diseases, as well as the potential for laboratory accidents and intentional misuse of life sciences and biotechnology. For these reasons, it is vital for us to work together – across the health, security, and development sectors – to enhance biopreparedness, biosafety, and biosecurity globally, and to reinforce the norm against the development and use of biological weapons.
The United States has made it clear that the weaponization of biological agents and toxins is unacceptable. Unfortunately, we are concerned that some nations still possess biological weapons programs, while other nations as well as nonstate actors seek to acquire them. We are therefore determined to strengthen and revitalize the Biological Weapons Convention (BWC). As we look to the Ninth Review Conference, we urge all countries to take seriously the threat of biological weapons, and for the Review Conference to overcome differences and take urgent steps to guard against the development and use of biological weapons. We must explore novel measures to promote implementation, increase transparency, and enhance compliance; measures that address the biological weapons threat of today — and tomorrow. This will be challenging work; success will require delegations to break out of old all-or-nothing mindsets and build new habits of constructive cooperation. We must demonstrate, to the world and to each other, that our shared efforts are about achieving real-world results. That is why the United States will also be proposing immediate action at the Review Conference on a number of practical measures that will build capacity to counter biological threats and benefit BWC members. The United States is committed to working with all States Parties to strengthen the BWC, and with all responsible nations to end the development of biological weapons and the threat they pose. Through collective action to counter all manner of biological threats – naturally occurring, accidental, and deliberate – together we can achieve global health security for everyone, everywhere.
ALL THINGS COVID-19
Effectiveness of Public Health Measures in Reducing the Incidence of COVID-19, SARS-CoV-2 Transmission, and COVID-19 Mortality: Systematic Review and Meta-Analysis
The objective of a new study published in The BMJ was to review the evidence on the effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and COVID-19 mortality. The study was designed as a systematic review and analysis, which included observational and interventional studies that assessed the effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality. The main outcome measure was incidence of covid-19. Secondary outcomes included SARS-CoV-2 transmission and covid-19 mortality. DerSimonian Laird random effects meta-analysis was performed to investigate the effect of mask wearing, handwashing, and physical distancing measures on incidence of COVID-19. Pooled effect estimates with corresponding 95% confidence intervals were computed, and heterogeneity among studies was assessed using Cochran’s Q test and the I2 metrics, with two tailed P values. 72 studies met the inclusion criteria, of which 35 evaluated individual public health measures and 37 assessed multiple public health measures as a “package of interventions.” Eight of 35 studies were included in the meta-analysis, which indicated a reduction in incidence of COVID-19 associated with, mask wearing, and physical distancing. Owing to heterogeneity of the studies, meta-analysis was not possible for the outcomes of quarantine and isolation, universal lockdowns, and closures of borders, schools, and workplaces. The effects of these interventions were synthesized descriptively. This systematic review and meta-analysis suggests that several personal protective and social measures, including handwashing, mask wearing, and physical distancing are associated with reductions in the incidence covid-19. Public health efforts to implement public health measures should consider community health and sociocultural needs, and future research is needed to better understand the effectiveness of public health measures in the context of COVID-19 vaccination. Read the article here.
The Government’s Preparedness for the COVID-19 Pandemic: Lessons for Government on Risk Management
The scale and nature of the COVID-19 pandemic and the government’s response are without precedent in recent history. Many people have died, and many lives, families and businesses have been adversely affected. By the end of July 2021, the estimated lifetime cost of measures announced as part of the government’s response was £370 billion. Like many other governments across the world, the UK government was underprepared for a pandemic like COVID-19. It will need to learn lessons from its preparations for and handling of whole-system risks, which will include making judgements on what level of preparations is appropriate.
The Cabinet Office, through its Civil Contingencies Secretariat (CCS), is responsible for coordinating the government’s planning for, and response to, major emergencies. Individual departments and other public sector organizations are responsible for identifying and managing risks in line with their desired risk appetite, including relevant national risks allocated to them by the Cabinet Office. For example, the Department of Health & Social Care is responsible for planning for the health and social care impacts of health-related risks. All departments are responsible for planning for emergencies that would have significant consequences in their areas of remit.
A new report sets out the UK government’s risk analysis, planning, and mitigation strategies prior to the arrival of the COVID-19 pandemic, with the aim of drawing out wider learning for the government’s overall risk management approach. It does not cover local-level risk planning, wider aspects of resilience planning or top-level disaster response procedures. It also does not cover the government’s response to COVID-19 or how prepared it was for subsequent waves of the pandemic.
This pandemic has exposed a vulnerability to whole-system emergencies – that is, emergencies that are so broad that they engage the entire system. Although the government had plans for an influenza pandemic, it did not have detailed plans for many non-health consequences and some health consequences of a pandemic like COVID-19. There were lessons from previous simulation exercises that were not fully implemented and would have helped prepare for a pandemic like COVID-19. There was limited oversight and assurance of plans in place, and many pre-pandemic plans were not adequate. In addition, there is variation in capacity, capability and maturity of risk management across government departments.
The pandemic has highlighted the need to strengthen the government’s end‑to‑end risk management process to ensure that it addresses all significant risks, including interdependent and systemic risks. This will require collaboration on risk identification and management not only across government departments and local authorities, but also with the private sector and internationally. For whole‑system risks the government needs to define its risk appetite to make informed decisions and prepare appropriately so that value for money can be protected. The pandemic has also highlighted the need to strengthen national resilience to prepare for any future events of this scale, and the challenges the government faces in balancing the need to prepare for future events while dealing with day-to-day issues and current events. Read the report here.
Experimental Chewing Gum Reduces Virus in Saliva
An experimental chewing gum containing a protein that “traps” coronavirus particles could limit the amount of virus in saliva and help curb transmission when infected people are talking, breathing or coughing, researchers believe. The gum contains copies of the ACE2 protein found on cell surfaces, which the virus uses as a gateway to break into cells and infect them. In test-tube experiments using saliva and swab samples from infected individuals, virus particles attached themselves to the ACE2 “receptors” in the chewing gum. As a result, the viral load in the samples fell by more than 95%, the research team from the University of Pennsylvania reported in Molecular Therapy. The gum feels and tastes like conventional chewing gum, can be stored for years at normal temperatures, and chewing it does not damage the ACE2 protein molecules, the researchers said. Using gum to reduce viral loads in saliva, they suggest, would add to the benefit of vaccines and would be particularly useful in countries where vaccines are not yet available or affordable.
PREPARING FOR THE NEXT PANDEMIC
The World Together
In a consensus decision aimed at protecting the world from future infectious diseases crises, the World Health Assembly agreed to kickstart a global process to draft and negotiate a convention, agreement or other international instrument under the Constitution of the World Health Organization to strengthen pandemic prevention, preparedness and response.
The Health Assembly met in a Special Session, the second-ever since WHO’s founding in 1948, and adopted a sole decision titled: “The World Together.” The decision by the Assembly establishes an intergovernmental negotiating body (INB) to draft and negotiate a WHO convention, agreement, or other international instrument on pandemic prevention, preparedness and response, with a view to adoption under Article 19 of the WHO Constitution, or other provisions of the Constitution as may be deemed appropriate by the INB.
Article 19 of the WHO Constitution provides the World Health Assembly with the authority to adopt conventions or agreements on any matter within WHO’s competence. The sole instrument established under Article 19 to date is the WHO Framework Convention on Tobacco Control, which has made a significant and rapid contribution to protecting people from tobacco since its entry into force in 2005.
Under the adopted decision, the INB will hold its first meeting by 1 March 2022 (to agree on ways of working and timelines) and its second by 1 August 2022 (to discuss progress on a working draft). It will also hold public hearings to inform its deliberations; deliver a progress report to the 76th World Health Assembly in 2023; and submit its outcome for consideration by the 77th World Health Assembly in 2024.
World Commits to A Pandemic Response Pact: What’s Next
As researchers scrambled this week to learn more about Omicron, the latest SARS-CoV-2 coronavirus variant of concern, world leaders met to negotiate a way of ensuring that a crisis on the scale of the COVID-19 pandemic never happens again. The biggest decision made at the assembly is to collectively develop an accord, agreement or other ‘new instrument’ to govern pandemic response, including ensuring the equitable distribution of diagnostics, drugs and vaccines. A measure outside of the IHRs is helpful, experts say, because those regulations do not oversee vaccines and other means of fighting pathogens.
International accords — or other treaty-adjacent frameworks — typically take years to become reality, and the process for this one is expected to continue until at least 2024. The pivotal decision by the WHO’s 194 member states at this assembly to move forward with a “new instrument” marks the first step. The European Council’s Michel has said that a treaty would be a prime way to ensure the equitable distribution of vaccines and other medical countermeasures, such as protective equipment and diagnostic tests. One way to coax wealthy countries to share goods might be to link the action with sharing data, says Suerie Moon, a global health researcher at the Graduate Institute for International and Development Studies in Geneva.
Revisions to the IHRs will probably be debated at the World Health Assembly meeting next May, and amendments might even be adopted by the end of next year. But a pandemic accord or other such tool will take at least another three years.
Global and Community Health Faculty Member Shares Insight on Pandemic Preparedness in the Middle East in a New Publication
Amira Roess, professor in the College’s Department of Global and Community Health, says that while several Middle Eastern countries had preparedness plans in place prior to the COVID-19 pandemic, the region’s response shows that the implementation plans remain underdeveloped and under-resourced.
In “How Can the Middle East Better Prepare for the Pandemics of the Future?”, Roess notes that while the COVID-19 pandemic highlighted the global economic toll of emerging highly infectious pathogens, it has not yet resulted in long-lasting or meaningful investments in public health systems. She advocates for significant investments over the next five years in the region’s public health system workforce and strategic technological enhancements.
“Without thoughtful, long-term investment in public health preparedness, the mistakes of the past will be repeated,” Roess writes.
Roess’s piece is a chapter in Thinking MENA Futures from the Middle East Institute’s Strategic Foresight Initiative. The publication maps out possible futures for the Middle East and North Africa (MENA) region by drawing insight on key issues and trends from experts. The publication covers everything from economic development and the future of work to climate change adaptation and public health.
Roess is a nonresident scholar at the Middle East Institute, a nonpartisan think tank providing insight and policy analysis on matters in the Middle East. Thinking MENA Futures is available on the institute’s website.
New NTI | bio Report Recommends Actions to Prevent and Respond to High-Consequence Biological Threats
A new NTI | bio report was released on the margins of the Biological Weapons Convention Meeting of States Parties, “Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats,” offers actionable recommendations for the international community to bolster prevention and response capabilities for high-consequence biological events.
The report, written by NTI | bio Senior Fellow Dr. Jaime M. Yassif, Dr. Kevin P. O’Prey, and Christopher R. Isaac, summarizes key findings and recommendations from a March 2021 tabletop exercise on high-consequence biological threats, jointly hosted by NTI and the Munich Security Conference. This report, and the exercise that informed it, are the third in a series of collaborations between NTI and the Munich Security Conference—which have focused on reducing global catastrophic biological risks and building stronger systems for pandemic prevention and response.
The 2021 tabletop exercise included 19 senior leaders and experts from across Africa, the Americas, Asia, and Europe with decades of combined experience in public health, biotechnology industry, international security, and philanthropy. Exercise participants were asked to engage with a fictional scenario that portrayed a deadly, global pandemic involving an unusual strain of monkeypox virus that spread globally over 18 months. Ultimately, the scenario revealed that the initial outbreak had been caused by a terrorist attack using a pathogen engineered in a laboratory with inadequate biosafety and biosecurity provisions and weak oversight. By the end of the exercise, the fictional pandemic resulted in more than three billion cases and 270 million fatalities worldwide.
The report authors developed a set of concrete recommendations for the international community based on the key findings from the exercise discussion. The recommendations include:
- Bolster international systems for pandemic risk assessment, warning, and investigating outbreak origins
- Develop and institute national-level triggers for early, proactive pandemic response
- Establish an international entity dedicated to reducing emerging biological risks associated with rapid technology advances
- Develop a catalytic global health security fund to accelerate pandemic preparedness capacity building in countries around the world
- Establish a robust international process to tackle the challenge of supply chain resilience
Read the report here.
EVENTS
2021 Global Health Security Index: Advancing Collective Action and Accountability Amid Global Crisis
COVID-19 continues to disrupt lives and livelihoods, stress health systems, and exhaust social protections and government budgets—and it will not be the last global health emergency the world will face. The need for durable national health capacities and political and social environments that foster effective prevention and response measures has never been clearer.
Join the Nuclear Threat Initiative and the Johns Hopkins Center for Health Security for the launch of the 2021 Global Health Security Index on 8 December 2021 at 9 AM EST. The GHS Index is a comprehensive assessment that provides a benchmark for capacities to prevent, detect, and respond to epidemics and pandemics across 195 countries. Register here.
The Athena Agenda: Executing the Apollo Program for Biodefense
The Bipartisan Common on Biodefense published a baseline report in 2015, A National Blueprint for Biodefense: Leadership and Major Reform Needed to Optimize Efforts, which warned that the United States was inadequately prepared for biological threats. Six years later, the US experience with COVID-19 continues to validate our original findings. The Commission’s January 2021 report, The Apollo Program for Biodefense: Winning the Race Against Biological Threats, details an ambitious goal-directed program to develop and deploy the technologies needed to defend against all biological threats, empower public health, and prevent pandemics within just ten years. Since the release of this report, the pandemic continues to cause devastation throughout the United States and the world. Likewise, the risk of an accidental or deliberate release of even deadlier pathogens continues to rise. The past year has only emboldened the idea that we cannot let a pandemic like the one we are facing, or something worse, ever happen again.
The Commission will convene an in-person meeting, The Athena Agenda: Executing the Apollo Program for Biodefense, to provide a better understanding of ongoing federal efforts to implement The Apollo Program for Biodefense, the role of the private sector in implementing The Apollo Program for Biodefense, how the public and private sectors can fully implement The Apollo Program for Biodefense within ten years. Register here.
Pandora Report: 11.19.2021
Anti-vaccine influencers on social media are pushing bogus methods to “undo” the vaccine. A COP26 special report provides a health argument for climate action. The Pandora Report will be taking Thanksgiving week off to safely spend time with family and friends, and we wish you a lovely holiday!
How to Make Holiday Gatherings Safer: 6 Things to Keep in Mind
According to Dr. Saskia Popescu and Dr. Syra Madad, compared to the holidays in 2020, this year’s celebration season has two advantages: (1) we have safe and effective vaccines against COVID-19 and (2) we’re much more attuned to risk reduction measures like the availability of at-home testing, ventilation, and better masks that can make any type of gathering safer. Popescu and Madad urge us to keep six things in mind as we gather for the upcoming holidays: vaccination, testing, mask, people, place, and time and space.
Antibiotic-Resistant Infections Could Be a New “Hidden Pandemic,” UK Experts Warn
Experts in the UK are warning that antibiotic-resistant infections are the next big concern as a “hidden pandemic.” The World Health Organization describes this risk as “one of the biggest threats to global health, food security, and development today.” In the UK, in 2020, one in five people with a bloodstream infection had a resistant one. As winter nears, experts fear that there will be another increase in antibiotic-resistant infections. The UK Health Security Agency has cautioned that the data suggest “resistant infections are likely to rise in the post-pandemic years and will require ongoing action.”
COP26
COP26 Special Report on Climate Change and Health
The 10 recommendations in the COP26 Special Report on Climate Change and Health propose a set of priority actions from the global health community to governments and policy makers, calling on them to act with urgency on the current climate and health crises.
The recommendations were developed in consultation with over 150 organizations and 400 experts and health professionals. They are intended to inform governments and other stakeholders ahead of the 26th Conference of the Parties (COP26) of the United Nations Framework Convention on Climate Change (UNFCCC) and to highlight various opportunities for governments to prioritize health and equity in the international climate movement and sustainable development agenda. Each recommendation comes with a selection of resources and case studies to help inspire and guide policymakers and practitioners in implementing the suggested solutions. Read the report here.
‘COP26 Hasn’t Solved the Problem’: Scientists React to UN Climate Deal
Government ministers at the 26th United Nations Climate Change Conference of the Parties (COP26) have reached a deal on further steps to reduce greenhouse-gas emissions after discussions overran by 24 hours. On 13 November, representatives from nearly 200 countries agreed the final text of the deal, which pledges further action to curb emissions, more frequent updates on progress and additional funding for low- and middle-income countries. Researchers have expressed relief that the meeting did produce an agreement, but some left COP26 dissatisfied at the lack of stronger commitments to reduce emissions, and failure to agree “loss and damage” finance for countries that are vulnerable to climate change. “COP26 has closed the gap, but it has not solved the problem,” says Niklas Hoehne, a climate researcher at Wageningen University in the Netherlands. Countries now need to come forward with more ambitious pledges to tackle climate change, he adds. Read more about scientists’ reactions to COP26 here.
Here’s What World Leaders Agreed To — And What They Didn’t — At the UN Climate Summit
After two weeks of intense negotiations in Glasgow, world leaders signed off on a new climate change agreement. Some nations pledged to impressive cuts to pollution, but many others “did not agree to rein in emissions fast enough for the world to avoid the worst damage from climate-driven storms, heat waves and droughts.” If countries stick to their promises, experts say that those goals may still be in reach. By 2030, emissions need to be cut by 45% to limit warming to 1.5 degrees Celsius by 2100 (2.7 degrees Fahrenheit). Over 100 countries committed at the summit to cut methane emissions 30% by 2030. In a surprise statement, the US and China agreed to work together to “strengthen and accelerate climate action and cooperation” in the near-term. It was proposed that wealthier nations compensate developing nations for climate change-related “loss and damage.” This proposal ran into a brick wall, but “discussions will begin between nations about how loss and damage funding might work.” Wealthy nations have also not provided the promised $100 billion of funding to support climate action.
WHO & SOCIAL SCIENCE
SAGO Has a Politics Problem, And WHO Is Ignoring It
The World Health Organization’s (WHO) Scientific Advisory Group on the Origins of Novel Pathogens (SAGO) has recently been established to “define and guide studies into the origins [of Novel Pathogens]” and “advise WHO on prioritizing studies and field investigations into [Novel Pathogens].” In both of these, an attention to political questions like “which pathogens deserve investigation?” and “how should countries’ possible pathogen origins be prioritized?” will need to be addressed.
However, arguments have been made by WHO that SAGO should “follow the science” and “avoid politicization.” There is a clear tension here. The statement to “avoid politicization” is a political act in itself. It is an act that suggests states, government, and citizens have no business in holding science to account. In turn it is an act that both recognizes the role and importance of politics, but sees the answer as doing nothing about it. Politics is framed as a problem—a major stumbling block to both pandemic preparedness and response, and for science to do its work—but one best avoided rather than understood. Political expertise is reduced to the important work of diplomacy or political communication. There is also an assumption that all political engagement means partisan or geo-politics, which is a misnomer. Politics is located at all levels, from the micropolitics of the Wuhan laboratory to the geopolitics of the G7 and UN systems. The publication of the membership of SAGO shows a lack of attention to expertise in the social sciences, and politics in particular. This is sure to cause problems in two domains core to the functioning of SAGO: the politics of pathogenic origins, and the politics of global investigations. Read the article about the WHO and SAGO here.
Joint Research Centre and World Health Organization Join Forces to Use Behavioral Insights for Public Health
The European Commission’s Joint Research Centre (JRC) and the World Health Organization (WHO) concluded a Collaborative Research Arrangement that aims to mainstream behavioral insights into public health programs and policies worldwide. Behavioral insights can help improve understanding on how and why people behave in ways that affect their health, and help design policies and services that address behavioral factors for improved physical and mental well-being.
The Commission, through the JRC, will assist WHO in expanding its behavioral insights for health program. Both organizations will agree on specific areas of focus, which would include issues like non-communicable diseases, anti-microbial resistance and the use of behavioral insights to increase the capacity of health workforce.
This Collaborative Research Arrangement builds on the priority placed by European Commission’s President Ursula von der Leyen on public health. It will contribute to building the European Health Union and promoting reforms in health governance in the EU and worldwide. The JRC’s Competence Centre on Behavioral Insights, which works to support EU policymaking with evidence on human behavior, will drive the new collaboration.
ALL THINGS COVID-19
COVID Vaccine Holdouts Are Caving to Mandates – Then Scrambling to “Undo” Their Shots
A popular TikTok video posted by a Dr. Carrie Madej detailed the ingredients for a bath she claims will “detox” the vaccine for people who caved to the COVID-19 vaccine mandates. Though the ingredients for this supposed detox bath are mostly not harmful, its effects are completely fictional. This is just one of several examples of bogus methods to undo the vaccine posted by anti-vaccine influencers on social media. Angela Rasmussen, a virologist, stated that the “lifesaving vaccination process” begins as soon as a person is injected, and it cannot be counteracted.
How COVID Might Sow Chaos in the Brain
“Brain fog” is not a formal medical descriptor. But it aptly describes an inability to think clearly that can turn up in multiple sclerosis, cancer or chronic fatigue. Recently, the condition has grabbed headlines because of reports that it afflicts those recovering from COVID-19.
COVID’s brain-related symptoms go beyond mere mental fuzziness. They range across a spectrum that encompasses headaches, anxiety, depression, hallucinations and vivid dreams, not to mention well-known smell and taste anomalies. Strokes and seizures are also on the list. One study showed that more than 80 percent of COVID patients encountered neurological complications.
The mystery of how the virus enters and then inhabits the brain’s protected no-fly zone is under intensive investigation. At the 50th annual meeting of the Society for Neuroscience, or SFN (held in virtual form this month after a pandemic hiatus in 2020), a set of yet-to-be-published research reports chronicle aspects of the COVID-causing SARS-COV-2 virus’s full trek in the brain—from cell penetration, to dispersion among brain regions, to disruption of neural functioning. Read more about COVID’s effects on the brain here.
Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-Analysis
Are race and ethnicity–based COVID-19 outcome disparities in the United States associated with socioeconomic characteristics? In this systematic review and meta-analysis of 4.3 million patients from 68 studies, African American, Hispanic, and Asian American individuals had a higher risk of COVID-19 positivity and ICU admission but lower mortality rates than White individuals. Socioeconomic disparity and clinical care quality were associated with COVID-19 mortality and incidence in racial and ethnic minority groups. In this study, members of racial and ethnic minority groups had higher rates of COVID-19 positivity and disease severity than White populations; these findings are important for informing public health decisions, particularly for individuals living in socioeconomically deprived communities. Read the full article here.
Vaccine Development: Capabilities and Challenges for Addressing Infectious Diseases
The CARES Act requires the Government Accountability Office (GAO) to look at the government’s response to the COVID-19 pandemic, including vaccine development. A new report discusses technologies, approaches, and associated challenges for vaccine (1) research and development, (2) testing, and (3) manufacturing, as well as (4) the economic factors that affect vaccine investment. Vaccines protect people from disease by preparing the body to respond to an infection. Vaccinations are a key part of individual and community health, but vaccine development remains complex and costly. Innovative technologies and approaches, such as those identified in this report, may enhance the nation’s ability to respond to infectious diseases. For example, reverse vaccinology and next generation platforms—combined with existing research—helped researchers develop some COVID-19 vaccines more quickly and effectively.
However, key challenges may hinder the adoption of these innovative technologies and approaches. Some promising technologies face issues and challenges such as inherent technical limitations and high cost. For example, organ chips may facilitate testing, but they are not yet able to replicate many of the complex functions of the human immune system. Similarly, single-use systems may increase the flexibility of vaccine manufacturing facilities, but may require extensive testing to ensure that they do not negatively affect the resulting vaccine. Further, economic challenges may hinder vaccine development. Experts attribute underinvestment in vaccines to market failures (i.e., market interactions that fall short of what would have been socially beneficial). For example, vaccines benefit those who are vaccinated, and, to some degree, those who are not. This additional benefit is not captured in the price, which reduces return on vaccine investment.
Overall, vaccine development is still difficult, complex, and costly. But GAO identified 16 innovative technologies and approaches that may enhance the nation’s ability to respond to high-priority infectious diseases. Read the report here.
Pandemic and Seasonal Influenza Vaccine Preparedness Collection
While the world responds to the COVID-19 pandemic, novel influenza viruses continue to be a constant pandemic threat. These viruses, which could appear at any time, can lead to circumstances and ramifications similar to or worse than the current experiences resulting from the COVID-19 pandemic. The global response to COVID-19 has expanded what is possible for rapid pandemic response in several areas, including vaccine research and development, more resilient supply chains, public health interventions and the need for global coordination. The reports in this collection explore how these unprecedented actions could inform and advance future pandemic and seasonal influenza vaccine preparedness efforts. The collection features four reports, addressing different areas of pandemic and seasonal influenza vaccine preparedness and response:
- Vaccine Research and Development to Advance Pandemic and Seasonal Influenza Preparedness and Response: Lessons from COVID-19
- Public Health Lessons for Non-Vaccine Influenza Interventions: Looking Past COVID-19 Countering the Pandemic Threat Through Global Coordination on Vaccines: The Influenza Imperative
- Globally Resilient Supply Chains for Seasonal and Pandemic Influenza Vaccines
Read the collection here.
EVENTS
The Independent Panel for Pandemic Preparedness and Response: Six Months On, What Has Changed?
In May 2021, the Independent Panel for Pandemic Preparedness and Response released its main report, calling for urgent action to end the pandemic, and for leadership to implement a package of international reforms to make COVID19 the last pandemic of such devastation. Six months later, there has been some progress, but is it urgent and cohesive enough? Will it result in the universal health protection that people worldwide need?
The key areas to reform pandemic preparedness and response are: effective leadership, inclusive governance, finance, ensuring equitable access to global public goods like vaccines, and strengthening WHO – including through a pandemic treaty.
The former Co-Chairs of the Independent Panel, HE Ellen Johnson Sirleaf and the Rt. Honourable Helen Clark, have prepared a six-month progress report which includes solutions and next steps. How can we seize the moment to strengthen international, regional, national, and local systems for pandemic preparedness and response?
Please join on Monday November 22nd at 12 GMT, when the former Co-Chairs of the Independent Panel for Pandemic Preparedness and Response, the Right Honourable Helen Clark and Her Excellency Ellen Johnson Sirleaf will present their new assessment of progress and urgent actions required to end the COVID-19 pandemic and prevent another of such devastation. Register here.
Report Launch: Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats
The Nuclear Threat Initiative (NTI) and the Munich Security Conference (MSC) brought together senior leaders and experts from across Africa, the Americas, Asia, and Europe in March 2021 for a scenario-based tabletop exercise on reducing high-consequence biological threats. The virtual exercise—which convened leaders in public health, biotechnology industry, international security, and philanthropy— examined critical gaps in national and international biosecurity and pandemic preparedness, and explored opportunities to improve capabilities to prevent and respond to high-consequence biological events.
Join NTI for the launch of the report, Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats, on 23 November at 7:45 AM EST. The report summarizes key findings and actionable recommendations derived from the 2021 tabletop exercise. The event will be chaired by NTI|bio Interim Vice President Dr. Margaret A. Hamburg and feature remarks from NTI|bio Senior Fellow Dr. Jaime Yassif, as well as senior international leaders in biotechnology industry and public health. This event is being hosted as a side event on the margins of the Biological Weapons Convention Meeting of States Parties. Register here.
Online Conference – One Health Intelligence: From Information to Action
On 29 November, the One Health Intelligence: From Information to Action conference will be held online. Speakers include experts from Ecohealth International, Department of Veterinary and Animal Sciences at University of Copenhagen, Vétérinaires sans Frontières Suisse, and more. Register here.
2021 Global Health Security Index: Advancing Collective Action and Accountability Amid Global Crisis
COVID-19 continues to disrupt lives and livelihoods, stress health systems, and exhaust social protections and government budgets—and it will not be the last global health emergency the world will face. The need for durable national health capacities and political and social environments that foster effective prevention and response measures has never been clearer.
Join the Nuclear Threat Initiative and the Johns Hopkins Center for Health Security for the launch of the 2021 Global Health Security Index on 8 December 2021 at 9 AM EST. The GHS Index is a comprehensive assessment that provides a benchmark for capacities to prevent, detect, and respond to epidemics and pandemics across 195 countries. Register here.
The Athena Agenda: Executing the Apollo Program for Biodefense
The Bipartisan Common on Biodefense published a baseline report in 2015, A National Blueprint for Biodefense: Leadership and Major Reform Needed to Optimize Efforts, which warned that the United States was inadequately prepared for biological threats. Six years later, the US experience with COVID-19 continues to validate our original findings. The Commission’s January 2021 report, The Apollo Program for Biodefense: Winning the Race Against Biological Threats, details an ambitious goal-directed program to develop and deploy the technologies needed to defend against all biological threats, empower public health, and prevent pandemics within just ten years. Since the release of this report, the pandemic continues to cause devastation throughout the United States and the world. Likewise, the risk of an accidental or deliberate release of even deadlier pathogens continues to rise. The past year has only emboldened the idea that we cannot let a pandemic like the one we are facing, or something worse, ever happen again.
The Commission will convene an in-person meeting, The Athena Agenda: Executing the Apollo Program for Biodefense, to provide a better understanding of ongoing federal efforts to implement The Apollo Program for Biodefense, the role of the private sector in implementing The Apollo Program for Biodefense, how the public and private sectors can fully implement The Apollo Program for Biodefense within ten years. Register here.
Pandora Report: 11.12.2021
Happy Veterans Day and thank you to all who served! COVID-19 has clearly demonstrated that the United States is vulnerable to biological threats of pandemic scale, and, unfortunately, this awareness has come at exceptionally high costs when calculated in lives lost and the severely compromised welfare of American citizens. The COVID-19 pandemic has led to renewed discussion of biological weapons and whether bad actors — both nations and terrorists — have refocused their attention on developing them.
Meet the PhD Biodefense Student and Counterproliferation Advisor Who Writes Sci-Fi and Spy Thrillers
Fiction writers are often asked what inspires their ideas. In the case of this important plot point, in the new book Interstellar Angel (An Astral Heat Romance) by Laura Navarre, the light-bulb moment for the story came during a real-life biodefense PhD class about genetically modified pathogens. That’s where she cooked up in her mind the fictional Valyrensis novicida, which, in the story, eradicates exactly 88 percent of the Valyrians, who are the galaxy’s leading race. The ensuing turmoil across the galaxy causes a pangalactic race war.
The novel, the first of a series, debuted on Amazon’s LGBTQ+ Science Fiction bestseller list when it was released in October. In a bit of apparent family competitiveness, Laura’s “sinister twin sister” Nikki has published The Russian Obsession, one of a trio of espionage thrillers rooted in the realities of high-tech intelligence.
Interesting family, yes? But wait: There’s a twist. Laura and Nikki Navarre are actually one and the same. Those are the noms de plume of Laura Schmidt Denlinger, a senior counterproliferation advisor and a PhD student at the Schar School of Policy and Government’s groundbreaking biodefense program.
By day, Denlinger is a Department of Energy National Laboratories employee on a long-term rotation to a sister US. government agency where she advances cutting-edge cooperative threat reduction work. Once you know what she does for a living, the idea of wiping out 88 percent of a galaxy’s population as detailed in her fiction isn’t so far-fetched. Read more here.
BRIEFER: Key US Initiatives for Addressing Biological Threats Part 6
The Nolan Center, an institute of the Council on Strategic Risks, is releasing its sixth briefer in its series Key US Initiatives for Addressing Biological Threats, which focuses on the US Department of Defense’s Defense Advanced Research Projects Agency (DARPA). Dr. Yong-Bee Lim, newly minted PhD from the Biodefense Graduate Program, was a co-author of this briefer. COVID-19, the disease caused by SARS-CoV-2, has clearly demonstrated that the United States is vulnerable to biological threats of pandemic scale. Unfortunately, this awareness has come at exceptionally high costs when calculated in lives lost and the severely compromised welfare of American citizens.
However, the pandemic has also reinforced the aphorism that necessity is the mother of invention – shining a light on numerous examples of governments making the impossible possible. In the midst of COVID-19, one such example can be seen in the forward-thinking work conducted by DARPA. Through heavy focus and investment in 2012 in a program called ADEPT:PROTECT, DARPA was instrumental in exploring the use of messenger RNA (mRNA) as a platform to deliver “antibody-making instructions” against specific diseases: the very technology that the United States leveraged through the $40 billion Operation Warp Speed to rapidly accelerate the creation, testing, production, and distribution of safe and effective COVID-19 vaccines around the globe.
As government agencies evaluate lessons from the ongoing pandemic, it is important to consider how to best leverage DARPA to address future biological threats and avoid strategic surprise. Further, it is important to delve into the organization itself in a bid to optimize its performance against rapidly-evolving biological threats of the future from natural and anthropogenic sources.
This is the focus of CSR’s sixth briefer in the series. In it, the authors highlight how DARPA has achieved past successes, and propose several recommendations to maximize the capabilities of DARPA for addressing biological threats:
- Strong leadership that focuses on high-risk, high-reward research is necessary to lead DARPA in addressing the most pressing threats to national security and Servicemembers.
- Have both top-down and bottom-up approaches with organizational structure.
- Improve funding mechanisms and sources to best allocate resources for promising research.
- Balance the high-churn that characterizes DARPA with extended timelines for DARPA Office Directors and Program Managers.
Read the sixth briefer here.
Biological Weapons in the “Shadow War”
Dr. Glenn Cross, an alumnus of the Biodefense Graduate Program, recently published an article in War on the Rocks about biological weapons. Do countries still need to worry about threats from biological weapons? The COVID-19 pandemic has led to renewed discussion of biological weapons and whether bad actors — both nations and terrorists — have refocused their attention on developing them. In a recent War on the Rocks article, Joseph Buccina, Dylan George, and Andy Weber argue that the “inadequate initial US response to COVID-19, coupled with new advances in biotechnology, could make biological weapons more appealing for US adversaries.” They add that China and Russia could use biological agents in a “low-boil” manner to undermine the United States as part of a “Shadow War,” a term first coined by Jim Sciutto, referring to a hybrid war, gray war, or non-linear war.
The specter of mass casualty biological weapons attacks — whether by nations or terrorists — is unrealistic. The United States should not overreact to the threat of biological weapons. Although the threat from biological weapons has not vanished, it is, in fact, at one of its lowest points since the Cold War’s end. Biological weapons are primarily a tool of assassination — largely for purposes of ensuring regime security in authoritarian states — and special forces operations. US policymakers should strengthen diplomatic and intelligence community efforts to protect the American people from this enduring — but manageable — threat. Read the article here.
The 2021 Report of the Lancet Countdown on Health and Climate Change: Code Red for a Healthy Future
The Lancet Countdown is an international collaboration that independently monitors the health consequences of a changing climate. Publishing updated, new, and improved indicators each year, the Lancet Countdown represents the consensus of leading researchers from 43 academic institutions and UN agencies. The 44 indicators of this report expose an unabated rise in the health impacts of climate change and the current health consequences of the delayed and inconsistent response of countries around the globe—providing a clear imperative for accelerated action that puts the health of people and planet above all else.
The 2021 report coincides with the UN Framework Convention on Climate Change 26th Conference of the Parties (COP26), at which countries are facing pressure to realise the ambition of the Paris Agreement to keep the global average temperature rise to 1·5°C and to mobilise the financial resources required for all countries to have an effective climate response. These negotiations unfold in the context of the COVID-19 pandemic—a global health crisis that has claimed millions of lives, affected livelihoods and communities around the globe, and exposed deep fissures and inequities in the world’s capacity to cope with, and respond to, health emergencies. Yet, in its response to both crises, the world is faced with an unprecedented opportunity to ensure a healthy future for all. Read the report here.
CLIMATE CHANGE
2021 WHO Health and Climate Change Survey Report
This report provides a vital snapshot of the overall progress that governments have made in the field of health and climate change to date, as well as insight into what work remains in order to protect their populations from the most devastating health impacts of climate change. The health and climate change country survey is conducted every three years and in addition to tracking global progress, the national data are presented in the health and climate change country profiles. 95 countries participated in the 2021 survey.
The survey is sent to the national health authorities, who in collaboration with other relevant ministries and stakeholders, provide updated information on key areas including: leadership and governance, national vulnerability and adaptation assessments, emergency preparedness, disease surveillance, adaptation and resilience measures, climate and health finance, and mitigation in the health sector. Regular updates on key health and climate change indicators provide insight into the implementation of policies and plans, the status of assessments of health vulnerability and capacity to respond to climate change and better understand the barriers to achieving health adaptation and mitigation priorities.
The 2021 global survey report provides an update to the 2017/2018 survey, and was published at the COP26 UN climate conference in November 2021. Read the report here.
This Is What the World Looks Like If We Pass the Crucial 1.5 Degree Climate Threshold
One point five degrees Celsius is the metric heard most on the podiums at the United Nations Climate Change Conference (COP26) in Glasgow this year. The hope is that limiting the planet’s warming to 1.5 degrees Celsius (2.7 degrees Fahrenheit) by 2021, the world will halt severe climate disruptions that would further exacerbate hunger, drought, and conflict. This is not a new goal. At the 2015 climate negotiations in Paris, there was a push for “industrialized countries to improve on the 2-degree Celsius goal held at the time, since wealthier nations are responsible for most greenhouse gas emissions since the Industrial Revolution.” Scientists expect a number of problems if average global temperatures exceed the limit. The Great Barrier Reef, located off the coast of Australia and massive enough to be viewable from space, would shrink tremendously. In fact, at 1.5 degrees Celsius, 70-90% of the world’s coral reefs could die off, and at 2 degrees Celsius, 99% will likely be lost. A hotter atmosphere will produce more rainfall and stronger storms. The UN’s climate research group predicts that sea levels could rise an additional one to three feet over the next 80 years.
ALL THINGS COVID-19
The Unvaccinated Drive COVID-19 Infections in the US
Winter is coming and COVID-19 infections are likely to increased among both the vaccinated and unvaccinated. But, data from the Centers for Disease Control and Prevention (CDC) show that there is “a significant difference between both groups across all age cohorts in the likeliness to become infected with the coronavirus.” Indeed, in August and September of this year, the infection rates per 100,000 individuals were 6-10 times higher among the unvaccinated compared with vaccinated people from the same age group. Further, hospitalization rates were 10-15 times higher for unvaccinated versus vaccinated people. Vaccination coverage in the US increases with the age group: 86% of individuals 65 years or older are vaccinated. The graph below from Statista shows the weekly rates of COVID-19 cases in certain age groups within the US based on vaccination status.

COVID-19 Misinformation is Ubiquitous: 78% of the Public Believes or is Unsure About At Least One False Statement, and Nearly a Third Believe At Least Four of Eight False Statements Tested
According to a new KFF COVID-19 Vaccine Monitor report, over three-quarters of the US adult population believes or is uncertain about at least one of eight false statements regarding the COVID-19 pandemic or the COVID-19 vaccines. Sixty-four percent of unvaccinated adults either believe or are unsure about at least four of the eight false statements; among vaccinated adults, this drops to 19%. Almost half of Republicans believe or are unsure about four or more of the false statements, which is three times the figure for democrats. Sixty percent of adults say “they’ve heard that the government is exaggerating the number of COVID-19 deaths by counting deaths due to other factors and either believe it to be true (38%) or aren’t sure if it is true or false (22%).” Thirty-nine percent say “they’ve heard pregnant women should not get the COVID-19 vaccine and believe it to be true (17%) or aren’t sure (22%).” Finally, 31% say “they’ve heard that the vaccine has been shown to cause infertility and either believe it (8%) or aren’t sure if it’s true (23%).”

Rethinking Health Security After COVID-19
The COVID-19 pandemic has posed major challenges to existing systems of global health governance. Even countries considered leaders in health preparedness, notably the US and the UK, struggled to contain COVID-19 domestically and were unable to mount an effective international response. As a result, the world suffered over 4.4 million deaths and an estimated 4.4 per cent decline in global GDP in 2020 alone – the deepest global recession since the end of World War II. The economic and health impacts of the pandemic have, meanwhile, fallen disproportionately on the world’s most disadvantaged and vulnerable populations.
COVID-19 has therefore laid bare deep fissures in the current global health architecture and highlighted the need for urgent reform. One proposal for reducing the risk of future pandemics is to elevate public health as a national security priority. For decades, policymakers and experts have argued that the concept of national security should extend beyond state-centric, military-focused threats, to include infectious diseases and climate change. Accordingly, the US and UK governments, both erstwhile leaders in global health and biological preparedness, have committed to promoting health security as a framework for mitigating the threat of future pandemics. A health security approach, it has been argued, will increase attention, resources, and institutional capacity for dealing with health crises.
Yet the reflexive tendency to frame health risks in security terms has precluded serious examination of the assumptions and trade-offs underlying the health security paradigm. In this report, the authors contend that, while the security implications of pandemics are clear, the concept of health security distracts attention from the underlying determinants of health that exacerbate the effects of severe disease outbreaks and disproportionately affect the most vulnerable. Rather than adopting a securitised approach to infectious disease, COVID-19 should prompt world governments to focus on the wider determinants of health – such as universal health coverage and access to quality health care, among other health-related UN Sustainable Development Goals – as a way to ameliorate the impact of pandemics and other crises. The report challenges the following assumptions that undergird health security and proposes recommendations for an alternative approach. Read the report here.
How an Outbreak Became a Pandemic: A Chronological Analysis of Crucial Junctures and International Obligations in the Early Months of the COVID-19 Pandemic
Understanding the spread of SARS-CoV-2, how and when evidence emerged, and the timing of local, national, regional, and global responses is essential to establish how an outbreak became a pandemic and to prepare for future health threats. With that aim, the Independent Panel for Pandemic Preparedness and Response has developed a chronology of events, actions, and recommendations, from December, 2019, when the first cases of COVID-19 were identified in China, to the end of March, 2020, by which time the outbreak had spread extensively worldwide and had been characterised as a pandemic. Datapoints are based on two literature reviews, WHO documents and correspondence, submissions to the Panel, and an expert verification process. The retrospective analysis of the chronology shows a dedicated initial response by WHO and some national governments, but also aspects of the response that could have been quicker, including outbreak notifications under the International Health Regulations (IHR), presumption and confirmation of human-to-human transmission of SARS-CoV-2, declaration of a Public Health Emergency of International Concern, and, most importantly, the public health response of many national governments. The chronology also shows that some countries, largely those with previous experience with similar outbreaks, reacted quickly, even ahead of WHO alerts, and were more successful in initially containing the virus. Mapping actions against IHR obligations, the chronology shows where efficiency and accountability could be improved at local, national, and international levels to more quickly alert and contain health threats in the future. In particular, these improvements include necessary reforms to international law and governance for pandemic preparedness and response, including the IHR and a potential framework convention on pandemic preparedness and response. Read the article here.
How Trump’s Deal with Moderna Hampers the Global Vaccine Effort
Operation Warp Speed (OWS), a US government initiative established to accelerate the development of vaccines and therapeutics for COVID-19, funneled billions of dollars into Moderna in its race to get a vaccine to the public, but it came with a catch: no doses delivered to the United States could be shared with outside its borders. This deal made under the Trump administration has become a “key stumbling block in the global fight against COVID-19,” as priorities are shifting to vaccinate the rest of the world. Moderna has “refused to grant access to its technology to vaccine manufacturers serving the developing world and at multiple points resisted pleas to increase aid to the neediest countries, angering critics who say the Trump administration should have driven a tougher bargain with Moderna when it had the chance.” When the deal was struck, government officials were focused on getting vaccines for use at home, and the need to send them abroad was not considered. Robbie Silverman, the senior manager of private-sector advocacy at global justice organization Oxfam America, said that nine of out ten doses of the Moderna vaccine have gone to wealthy nations.
North Korean Hospital Mum on Cause of Death for 10 “Suspected” COVID-19 Patients
A hospital in the DPRK sent 10 patients with COVID-19 symptoms to an unheated area during freezing cold weather. The nature of their deaths was falsified to “maintain Pyongyang’s claim that the country is completely virus free.” The hospital claims that these patients perished from malnutrition, but the patients themselves complained of fever and were diagnosed with pneumonia. North Korea has instituted extensive measures to quell the spread of the novel coronavirus, including lock down on entire cities and counties, travel bans between provinces, and trade suspensions. Despite its crumbling medical and healthcare infrastructure, the nation claimed that its preventive measures worked and “not a single person was infected” in April 2020. But, the DPRK government tracks “suspected cases” of COVID-19 without ever confirming cases that present with the associated symptoms. The 10 aforementioned patients were immediately buried without providing explanation to the families. An anonymous source said, “No one has died from the coronavirus in North Korea because the public will never know about it. Hospitals announce those deaths are due to tuberculosis or flu.” In March 2021, an internal survey found about 13,000 “suspected cases” in North Hamgyong. As of September 21st, only 43,000 of the 25 million people in North Korea were tested for COVID-19, and not a single case was confirmed.
EVENTS
Schar School Open House
The Schar School will be a hosting virtual open house for the Master’s and Certificate Programs! These sessions will take place on 16 November at 6:30 PM EST. This online session will provide an overview of our master’s degree programs – such as the Biodefense Program – and our Graduate Admissions team will be available to answer questions about admissions requirements, application deadlines, and materials to prepare. By working closely with faculty who draw on world-class research and practical experience, the Schar School prepares students for a high-powered career in the public, private, and non-profit sectors. Register here.
Preventing the Next Pandemic—Leveraging Today’s Tools to Address the Biological Threats of the Future
We are at a critical point for preventing future pandemics and addressing biological sources of all origins. Many of the technologies needed are available today. However, challenges remain in garnering the resources to deploy existing tools broadly, ensuring that investments cover diverse solutions that create a healthy bio industrial base, and effectively fostering technologies that require additional research and development support. The Council on Strategic Risks (CSR) invites you to a webinar, “Preventing the Next Pandemic—Leveraging Today’s Tools to Address the Biological Threats of the Future,” on 15 November at 11:15 AM EST. The guest speakers are Dr. Vik Bajaj, the CEO and cofounder of Foresite Capital, and Dr. Luciana Borio, Senior Fellow for Global Health at the Council on Foreign Relations. Register here.
Hashing the Atom: Exploring Blockchain Solutions for Global Security
Join the Stimson Center’s Blockchain in Practice program for a two-day discussion on how distributed ledger technology (DLT) can help to secure the use and trade of nuclear, chemical, and other dual-use goods and technologies. The event will feature insights on how DLT solutions are not only demonstrating greater efficiencies in data management and business operations; but also, how DLT can be used to enhance nonproliferation and global security. Speakers will present a landscape of DLT solutions and highlight their experience with tech acceptance, adoption, and how DLT is building trust across organizations. The webinar is set for 17 – 18 November from 11 AM to 2 PM EDT each day. Register here.
Effective Chemical Supply Chain Security: Embracing Behavioral Change
The ongoing pandemic has changed the ways chemical manufacturers and distributors do business. Current issues like rapid commoditization, complex supply chains, aging assets, and increased need for dynamic operations planning make it more demanding than ever to achieve the productivity level that drives differentiation and innovation. With the overall global demand falling due to the pandemic, chemical and pharmaceutical producers and wholesalers have had to explore new avenues to revitalize the chemical trade and increase market responsiveness.
This trend has brought new security challenges and vulnerabilities to the industry as wholesalers, eager to compensate for early losses, sold to unvetted companies. State proliferators are masters at exploiting these vulnerabilities in the chemical industry for their Chemical Weapons programs and the development of fourth-generation agents. Hence proactive due diligence, customer vetting, and effective management of chemical supply chains are critical among all sectors. The new approach requires proper tools and procedures to mitigate pitfalls in chemical supply chains and encourage behavioral changes to broaden security awareness within organizations.
Join CRDF Global for a panel discussion exploring innovative chemical supply chain management methodologies and a practical approach to behavioral change led by Steve Hess, a chemical security and supply chain management consultant, and David Toddington, an IT and Law Enforcement expert and the founder of Toddington International. The webinar will take place on 16 November at 9 AM EST. Register here.
Pandora Report: 11.5.2021
The Intelligence Community (IC) assesses that SARS-CoV-2, the virus that causes COVID-19, probably emerged and infected humans through an initial small-scale exposure that occurred no later than November 2019 with the first known cluster of COVID-19 cases arising in Wuhan, China in December 2019. A team of scientists with specific expertise in climate modeling simulated the climate of Arrakis, the desert planet in Dune, to find out what such a world would be like. The Rockefeller Foundation will provide up to USD150 million in funding to the Pandemic Prevention Institute (PPI), a collaborative organization with a global network of partners committed to building data sets and analytics needed to detect, mitigate, and prevent pandemics.
Advancing Equity in Science & Technology Ideation Challenge
The White House Office of Science and Technology Policy (OSTP) is seeking ideas from the public about how to promote equity in STEM. The ideas must include at least one of these topics: people with disabilities; underrepresented racial and ethnic groups; institutional and academic settings; community centered research, participation, and engagement; women and people with gender-expansive identities; or open call (none of aforementioned topics apply). Previously, OSTP Director, Eric Lander, and OSTP Deputy Director for Science and Society, Alondra Nelson, hosted a series of 5 roundtable discussions, “The Time is Now: Advancing Equity in Science & Technology.” The directors engaged with participants about their expertise and experiences navigating careers in science and technology, trying to understand the complexity of issues. The goal is to build a STEM ecosystem that will enable everyone to succeed. More information on the most recent roundtable, “The COVID-19 Pandemic and Overlapping Crises for Women and People with Gender Expansive Identities in STEM,” can be found here. Other previous roundtables include Honoring Disability Pride Month; Diversity, Equity, Inclusion, and Anti-Racism; Emerging Models and Pathways for Success in (a) Institutional and Academic Contexts, and (b) Community-centered Research, Participation, and Engagement. To participate in the Advancing Equity in Science & Technology Ideation Challenge, see here.
The Nexus of Climate Change, Ecological Disruption, Stability, and Security
As the COVID-19 pandemic has made all too clear, are definition of national security is overdue. As we look to 2030, some of the biggest security risks the world faces will come not from states and governments alone, but also from complex transnational risks. This paper examines how climate change and ecological degradation, particularly deforestation and poor land use practices, intersect to undermine security and create instability. Within many states, these drivers are contributing to resource stress (e.g., food and water insecurity), governance strains, and internal migration. Between states, competition and nationalism are rising in response to these challenges. Extremists and violent non-state actors are also benefiting, which in turn threatens political stability and cross-border relations. Biological risks — stemming from greater human-animal interactions, and the accelerated emergence of infectious diseases — are woven through all of these interrelated issues.
A new paper begins by describing the relationship between forests, land use, and insecurity at the nexus of ecological disruption and climate change. It then proceeds to discuss how this nexus affects security in four categories: the intra-state, inter-state, and non-state actor levels, as well as looking at Indigenous and vulnerable populations through a lens of justice and equity. It concludes with concrete recommendations aimed at both managing existing risks while also preventing catastrophic risks in the longer-run. Dr. Yong-Bee Lim, newly minted PhD from the Biodefense Graduate Program, is one of the co-authors of this paper. Read it here.
Alternatives to Radioactive Materials: A National Strategy to Support Alternative Technologies May Reduce Risks of a Dirty Bomb
Radioactive material, which is dangerous if mishandled, is found in many medical and industrial applications. In the hands of terrorists, it could be used to construct a radiological dispersal device, or dirty bomb, that uses conventional explosives to disperse the material. Replacing technologies that use dangerous radioactive materials with safer alternatives may help protect people and reduce potential socioeconomic costs from remediation and evacuation of affected residents. Senate Report 116-102 included a provision for the Government Accountability Office (GAO) to review alternative technologies to applications that use radioactive materials. A new report examines (1) the potential for adopting alternative technologies in the United States for the six most commonly used medical and industrial applications; (2) factors affecting adoption of alternative technologies; and (3) federal activities relating to alternative technologies in the United States. GAO reviewed relevant documents to identify potential alternative technologies, conducted interviews with users of applications that employ radioactive material to identify factors affecting adoption of alternatives, and interviewed federal officials to discuss current federal activities relating to alternative technologies. Congress should consider directing an entity to develop a national strategy to support alternative technologies. The federal agencies involved in research and adoption of alternative technologies neither agreed nor disagreed with our matters for congressional consideration. Read the report here.
The ‘Echo Chamber’ of Syrian Chemical Weapons Conspiracy Theorists
The Assad regime in Syria has launched several attacks against its own people, including attacks using nerve agent sarin and chlorine gas. The regime has insisted it did not carry out these malicious activities. After a lethal sarin attack on Ghouta, Syria joined the Chemical Weapons Convention, yet their use of chemical weapons has continued. A cadre of small group and individuals in the West have “convinced themselves that one of the Middle East’s most oppressive regimes was the innocent victim of a plot to discredit it.” These deniers include university professors, retired spies, “independent” journalists, “anti-imperialists” and habitual conspiracy theorists. Eager to direct blame away from Assad, these deniers “claimed rebels were faking the attacks in an effort to falsely incriminate the regime and thus create a pretext for full-scale military intervention by Western powers.” Given the absence of credible evidence to support such a claim, they pointed to “confirmed examples from the past where deception had been used in warfare.” For example, they highlighted the “way false claims about weapons of mass destruction in Iraq had been used to build public support for the US-led invasion that toppled Saddam Hussein in 2003.” They insist that the reports of Syria’s chemical attacks are a similar form of deception with similar ends. “It was an argument that could be made to sound plausible, and the deniers exploited it relentlessly.” In reality, “laboratory tests on samples from the scene of attacks linked them to the regime’s own stockpile.”
Revisiting and Realizing the Promises of Synthetic Biology
Synthetic biology is a frontier field that employs science and engineering approaches to design biologically based parts, novel devices and systems as well as redesign existing, natural, biological systems. Its applications have expanded to almost every major industry. Potentially the broadest impact area is the manufacture of bio-based products and the numerous applications of these products in health and well-being, food and feed, industrial chemicals and biofuel applications.
The potential benefits of synthetic biology are manifold – but will they be distributed equitably? Wealthy nations have been at the forefront of synthetic biology and the livelihoods of those in developing and emerging economies have often been overlooked. As we learn to engineer the living world, how can we ensure it is a world in which we want to live? A new report from the World Economic Forum (WEF), Revisiting and Realizing the Promises of Synthetic Biology, looks at synthetic biology’s embodiment and advancement of equity, humility, sustainability and solidarity over time: four values that are important in realizing its future benefits and minimizing its potential negative consequences. It also provides recommendations on how policies could direct the future trajectory of synthetic biology to benefit all people and the planet. Read the report here.
Dune: We Simulated the Desert Planet of Arrakis to See If Humans Could Survive There

Dune, the epic series of sci-fi books by Frank Herbert, now turned into a movie of the same name, is set in the far future on the desert planet of Arrakis. Herbert outlined a richly-detailed world that, at first glance, seems so real we could imagine ourselves within it. However, if such a world did exist, what would it actually be like? A group of scientists with specific expertise in climate modeling simulated the climate of Arrakis to find out. They wanted to know if the physics and environment of such a world would stack up against a real climate model.
The mid-latitudes, where most people on Arrakis live, are actually the most dangerous in terms of heat. In the lowlands, monthly average temperatures are often above 50–60°C, with maximum daily temperatures even higher. Such temperatures are deadly for humans. The planet also gets very cold outside of the tropics, with winter temperatures that would also be uninhabitable without technology. Cities like Arrakeen and Carthag would suffer from both heat and cold stress, like a more extreme version of parts of Siberia on Earth which can have both uncomfortably hot summers and brutally cold winters. See their simulation here.
Ensuring an Effective Public Health Emergency Medical Countermeasures Enterprise
The US medical countermeasures (MCMs) enterprise is interconnected, complex, and dynamic. It includes public and private entities that (1) develop and manufacture new and existing MCMs; (2) ensure procurement, storage, and distribution of MCMs; and (3) administer, monitor, and evaluate MCMs. The interagency group the Public Health Emergency Medical Countermeasures Enterprise (PHEMCE) is the nation’s sole coordinating body, based in the US Department of Health and Human Services (HHS) with interagency participation and responsible for ensuring end-to-end MCM preparedness and response. PHEMCE’s authorities limit its membership to federal entities. However, it must also collaborate closely with nonfederal and private-sector partners and stakeholders, as they are the ultimate implementers of PHEMCE’s mission and develop, manufacture, distribute, and administer the MCMs over which PHEMCE has responsibility. These engagements must support the entire life cycle of MCM preparedness and response, where appropriate, including threat identification, development, manufacturing, deployment, distribution, administration, and evaluation. An effective national MCM enterprise requires a mechanism to coordinate and integrate the activities and expertise of the diverse landscape of federal agencies involved in these activities, and PHEMCE has the legislative mandate to serve that role.
Recognizing the important role of PHEMCE in coordinating the federal MCM preparedness and response activities, HHS’s Office of the Assistant Secretary for Preparedness and Response (ASPR) charged the National Academies of Sciences, Engineering, and Medicine with convening an ad hoc committee to evaluate PHEMCE’s policy and practices and make recommendations for a re-envisioned PHEMCE. The committee heard from knowledgeable experts reflecting a range of disciplines and experiences, including developers, producers, funders, responders, and federal, state, and local officials. The committee also examined government documents, including some first made public for this review.
Four priority areas of improvement emerged from committee deliberations: (1) articulating PHEMCE’s mission and role and explicating the principles guiding its operating principles and processes; (2) revising PHEMCE operations and processes; (3) collaborating more effectively with external public and private partners needed for the entire life cycle of MCMs, from research through use; and (4) navigating legal and policy issues. This report proposes recommendations for these four domains, re-envisioning PHEMCE to service its mandate to protect the nation in public health emergencies (PHEs). Read the report here.
ALL THINGS COVID-19
Office of the Director of National Intelligence: Updated Assessment on COVID-19 Origins
The Intelligence Community (IC) assesses that SARS-CoV-2, the virus that causes COVID-19, probably emerged and infected humans through an initial small-scale exposure that occurred no later than November 2019 with the first known cluster of COVID-19 cases arising in Wuhan, China in December 2019. In addition, the IC was able to reach broad agreement on several other key issues. We judge the virus was not developed as a biological weapon. Most agencies also assess with low confidence that SARS-CoV-2 probably was not genetically engineered; however, two agencies believe there was not sufficient evidence to make an assessment either way. Finally, the IC assesses China’s officials did not have foreknowledge of the virus before the initial outbreak of COVID-19 emerged. After examining all available intelligence reporting and other information, though, the IC remains divided on the most likely origin of COVID-19. All agencies assess that two hypotheses are plausible: natural exposure to an infected animal and a laboratory-associated incident.
The IC judges they will be unable to provide a more definitive explanation for the origin of COVID-19 unless new information allows them to determine the specific pathway for initial natural contact with an animal or to determine that a laboratory in Wuhan was handling SARS-CoV-2 or a close progenitor virus before COVID-19 emerged. The IC—and the global scientific community—lacks clinical samples or a complete understanding of epidemiological data from the earliest COVID-19 cases. If we obtain information on the earliest cases that identified a location of interest or occupational exposure, it may alter our evaluation of hypotheses.
China’s cooperation most likely would be needed to reach a conclusive assessment of the origins of COVID-19. Beijing, however, continues to hinder the global investigation, resist sharing information, and blame other countries, including the United States. These actions reflect, in part, China’s government’s own uncertainty about where an investigation could lead as well as its frustration the international community is using the issue to exert political pressure on China.
Read the report here.
COVID-19: Additional Actions Needed to Improve Accountability and Program Effectiveness of Federal Response
As the nation continues to respond to, and recover from, the COVID-19 pandemic, increases in COVID-19 cases in July, August, and September 2021, primarily due to the Delta variant of the virus, have hampered these efforts. From the end of July 2021 to September 23, 2021, the number of new cases reported each day generally exceeded 100,000, according to Centers for Disease Control and Prevention (CDC) data. This was a daily case count not seen since February 2021.
Meanwhile, COVID-19 vaccination efforts continue. As of September 23, 2021, about 64 percent of the US population eligible for vaccination (those 12 years and older), or almost 183 million individuals, had been fully vaccinated, according to CDC.
The government must remain vigilant and agile to address the evolving COVID-19 pandemic and its cascading impacts. Furthermore, as the administration implements the provisions in the COVID-19 relief laws, the size and scope of these efforts—from distributing funding to implementing new programs—demand strong accountability and oversight. In that vein, GAO has made 209 recommendations across its body of COVID-19 reports issued since June 2020. As of September 30, 2021, agencies had addressed 33 of these recommendations, resulting in improvements including increased oversight of relief payments to individuals and improved transparency of decision-making for emergency use authorizations for vaccines and therapeutics. Agencies partially addressed another 48 recommendations. GAO also raised four matters for congressional consideration, three of which remain open.
In a new report, Government Accountability Office (GAO) outlines 16 new recommendations, including recommendations related to fiscal relief funds for health care providers, recovery funds for states and localities, worker safety and health, and assessing fraud risks to unemployment insurance programs. GAO’s recommendations, if swiftly and effectively implemented, can help improve the government’s ongoing response and recovery efforts as well as help it to prepare for future public health emergencies. Read the report here.
G-20 Announces New Global Body to Respond to Future Pandemics, But Stops Short of Committing Funds
In October, leaders of the G-20 announced the establishment of a “global body for coordinating government responses to the next international pandemic, but the initiative faced immediate criticism because it appears to lack resources.” This new Joint Finance-Health Task Force is intended to “improve planning among the wealthiest nations to respond to pandemics with additional health-care resources and financing measures.” The G-20 includes the United States, France, Italy, Russia, Brazil, China, India, and Japan. Unfortunately, the announcement of the Task Force was sans a pledge of funding. G-20 health and finance ministers stated, “We remain committed to build on the lessons learned from the COVID-19 crisis to increase investment into longer term health capacity.” J. Stephen Morrison, director of the Global Health Policy Center at the Center for Strategic and International Studies (CSIS), shared his disappointment in the lack of funding despite “plenty of good analysis about what is failing and what needs to happen,” and that this initiative will “shift to a coalition of the willing approach.”
Navigating the World that COVID-19 Made: A Strategy for Revamping the Pandemic Research and Development Preparedness and Response Ecosystem
The actions being taken to respond to the COVID-19 crisis are writing the opening chapters to the story of how we will prepare for and respond to the next pandemic threat. To prevent the devastation that has accompanied the COVID-19 pandemic from happening again, we must not only identify the successes and failures that have emerged from the global response, we must also anticipate how our response has changed government, industry, and civil society priorities for the pandemic R&D and response ecosystem in order to confront to future threats.
Beyond its human and economic toll, the COVID-19 pandemic has also exposed and redefined the realities of the global vaccine R&D and response ecosystem in the following ways: (1) there is now widespread recognition that safe and effective vaccines provide unparalleled health, social, and economic benefits during a pandemic; COVID-19 has made it clear that most nations will not share scarce supplies of early vaccines and related inputs in a crisis; COVID-19 demonstrated that pandemics can be profitable for vaccine manufacturers; and geopolitics constrained COVID-19 response and threaten future global health security.
Any future pandemic pathogen that emerges will do so in a world changed by and aware of these realities. To ensure that these lessons are heeded and to prevent the devastation of the present crisis from repeating in the next pandemic, governments, international institutions, and private sector actors must immediately act to address gaps and explore opportunities at each step along the vaccine value chain. The measures to be taken should include: (1) develop and fund an inclusive strategy for the R&D of prototype vaccine candidates for future pandemics; (2) engage local government and donor financing and policy support to enable global vaccine manufacturing scale up; (3) create and support equitable financing, procurement, and allocation mechanisms to help end COVID-19 and prepare for the future; (4) strengthen cross-border trade, standardization, and supply chain transparency in order to expand vaccine manufacturing and access during a crisis; (5) build the systems needed to enable vaccine distribution, allocation, and uptake for the next pandemic; (6) and plan for global coordination of post-market research studies
Read the report here.
Operation Warp Speed: The Interagency and Public-Private Collaborations that Drove It
On Wednesday, October 27, the Council on Strategic Risks (CSR) hosted a webinar to discuss how the successes and challenges of Operation Warp Speed—the U.S. federal government’s effort to drive the development of COVID-19 vaccines—can be built upon in the future. This conversation on the future of rapid development, manufacturing, and delivery of medical countermeasures for biological threats was led by Christine Parthemore, CEO of CSR, and Andy Weber, Senior Fellow at CSR.
CSR hosted two incredible guests, Dr. Matt Hepburn and Dr. Monique K. Mansoura, who contributed a wealth of knowledge and insight on Operation Warp Speed and the partnerships that enabled it. Dr. Matt Hepburn is the Senior Advisor on Pandemic Preparedness to the Director of the Office of Science and Technology Policy. Prior to his role at OSTP, he directed COVID-19 Vaccine Development under the Countermeasures Acceleration Group, formerly known as Operation Warp Speed. Dr. Monique K. Mansoura is the Executive Director for Global Health Security and Biotechnology at The MITRE Corporation, where she focuses on the sustainability of the biodefense industrial base. At MITRE, Dr. Mansoura was also a part of the COVID-19 Healthcare Coalition, which brought together healthcare organizations, technology firms, nonprofits, academia, and startups in order to more effectively deploy healthcare resources.
In the webinar, Dr. Hepburn and Dr. Mansoura discussed how cooperation between the Department of Health and Human Services and the Department of Defense drove Operation Warp Speed, and how this is a stellar example that should be taken forward to nimbly solve future public health problems. In addition, the speakers emphasized that Operation Warp Speed was by no means perfect, and that lessons from what went wrong should be applied in future efforts. Dr. Hepburn and Dr. Mansoura also spoke on the American Pandemic Preparedness Plan, the importance of building a forward-looking bio-industrial policy, as recommended in MITRE’s 10-Point Action Plan: Sustaining A Biopharma Industrial Base for a More Secure Nation, and much more. Listen to their conversation here.
The Rockefeller Foundation Invests USD150 Million to Prevent Future Pandemics and Calls for Greater Collaboration to Build a Global Early Warning System
The Rockefeller Foundation will provide up to USD150 million in funding to the Pandemic Prevention Institute (PPI), a collaborative organization with a global network of partners committed to building data sets and analytics needed to detect, mitigate, and prevent pandemics. The Foundation also renewed its call for expanded collaboration to strengthen the global pandemic and epidemic intelligence ecosystem at the World Health Summit in October. This marks the next chapter in the Foundation’s more than 100-year history of using science and technology to improve public health and uplift humanity. Together with the World Health Organization’s Hub for Pandemic and Epidemic Intelligence in Berlin and the United Kingdom’s Global Pandemic Radar, the Pandemic Prevention Institute is helping transform global capability for stopping disease outbreaks.
The Pandemic Prevention Institute is also accelerating work to develop analytic tools and algorithms that detect early warning signals wherever they occur. Developing technology that sees and shares the signs of potential outbreaks, and supports sharing of those signals—instead of the data itself—is a crucial step to addressing data privacy and building an early warning system that works for all. Moving forward, the Pandemic Prevention Institute will actively seek new partners to define and invest in a common agenda through the RF Catalytic Capital, Inc. (RFCC), a charitable offshoot that The Rockefeller Foundation created in 2020 to enable foundations, governments, and other like-minded funders to combine their resources to build funding solutions for social impact and bring about transformational change. The RFCC, which is incubating the PPI, will eventually launch the Institute as a standalone entity.
LESSONS LEARNED FROM COVID-19 ACROSS THE GLOBE
Sweden During the Pandemic
Sweden represents an average European country as far as numbers of deaths during the first and second waves of the pandemic are concerned. During the third wave, mortality has been low and, up to now, Sweden has fared better than most countries in Europe. In the spring of 2020, Sweden chose a different path to many other countries, one based on a voluntary approach and personal responsibility rather than more intrusive measures. The majority of other countries, by contrast, made greater use of lockdowns or other intrusive regulatory interventions. Whether Sweden’s choice of path was reasonable, or whether it would have been better to introduce other types of measures to limit the spread of the virus, is a question the Commission will return to in its final report. To address that question, it is necessary to gain a better understanding of what information key decision-makers had as a basis for their assessments regarding disease prevention and control measures during the various phases of the pandemic. Several other aspects of Sweden’s handling of the crisis, moreover, remain to be investigated and assessed. These include, in particular, the impacts of the emergency on the economy and personal finances, and what capacity the Swedish machinery of government and its institutions had to manage a crisis. Only after that will the Commission be able to assess whether the path chosen by Sweden represented a reasonable balance between effective disease prevention and control and other interests. With answers to these questions, it will also be possible to better assess questions of responsibility.
The Commission has initiated a research programme – A Research Programme on COVID-19 in Sweden: Spread, Control and Impacts on Individuals and Society – based on very extensive gathering of data on medical and socio-economic outcomes, generally at the individual level, from a large number of sources. The Commission’s most important overall conclusions based on the review carried out to date and presented in this report include: (1) Sweden’s handling of the pandemic has been marked by a slowness of response; (2) Sweden’s pandemic preparedness was inadequate; and (3) its health care system has been able, at short notice, to adapt and to scale up care for people with COVID-19. Read the report here.
Russia: Six Lessons from One Pandemic
The Deputy Chairman of the Security Council of the Russian Federation D.A. Medvedev recently wrote an article on six key lessons learned from the COVID-19 pandemic. The first lesson of the pandemic is that threats must be taken seriously. And states must act proactively, not after the fact. The second lesson of the pandemic is that it can only be combated through the joint efforts of the international community. One by one, all are doomed to defeat. The third lesson of the pandemic is that the mutual trust of states is more important than commerce, ideology, and competition. The fourth lesson is that vaccine enforcement is not very effective, and education is needed. Fifth, every cloud has a silver lining. There are also positive aspects in the experience of the past two years, which, paradoxically, we owe to the pandemic. The main one is that we have learned to quickly respond to the most difficult and unpredictable challenges. Finally, this is a virus that will be with us for a long time. Read the article here.
EVENTS
2021 Global Conference on Health and Climate Change
The 2021 Global Conference on Health & Climate Change with a special focus on Climate Justice and the Healthy and Green Recovery from COVID-19 will convene at the margin of the COP26 UN climate change conference. The aim of the conference is to call on governments, businesses, institutions and financial actors to drive a green, healthy and resilient recovery from COVID-19. The Conference will support and highlight climate action recommendations that promote and protect health. It will also mobilize the rapidly growing movement of health professionals around the world who are now driving ambitious climate action. And it will generate cross-sectoral dialogue focused on integrated solutions for a green, just and healthy future. The conference has a fully developed hybrid program, with participation both online, and in-person at the Glasgow Caledonian University. The conference will be held tomorrow, 6 November, from 9 AM to 5:40 PM GMT. Register here.
Schar School Open House
The Schar School will be a hosting virtual open house for the Master’s and Certificate Programs! These sessions will take place on 16 November at 6:30 PM EST. This online session will provide an overview of our master’s degree programs – such as the Biodefense Program – and our Graduate Admissions team will be available to answer questions about admissions requirements, application deadlines, and materials to prepare. By working closely with faculty who draw on world-class research and practical experience, the Schar School prepares students for a high-powered career in the public, private, and non-profit sectors. Register here.
Biorisk Management Perspective: Then and Now Webinar
In partnership with the American Biological Safety Association’s (ABSA) Biosafety and Biosecurity Month, APHL is proud to provide this free webinar! This program will provide attendees with an overview of biorisk management innovation throughout the years. Participants will hear from three biosafety professionals on their perspectives of biosafety and biosecurity practices and discuss the potential role of biosafety professionals into the future. This program is intended for anyone who works in or supervises a public health, clinical and academic/research laboratory. These can include clinical and public health laboratory staff, microbiology students, veterinary microbiology laboratory workers, veterinarians, medical doctors, biosafety professionals, academia or biotech industry laboratory workers and research scientists. The webinar will be held on 1 and 8 November from 11:30 AM to 4 PM EST. Register here.
Preparing for the Next Pandemic
The term “post-pandemic world” has become ubiquitous ever since COVID vaccines were made widely available to the developed world. Yet, the bio-policy implications of a world coming out of the COVID-19 pandemic are rarely evaluated critically and holistically. COVID-19 pandemic points to the reality that a multifaceted approach is necessary to prevent future pandemics or, should the need arise again, how to stop them in their tracks. A webinar offered by CDRF Global brings together experts from different corners of the biosafety and biosecurity space to discuss lessons learned from the world’s response to COVID-19 and analyze policy pathways moving forward. The panel will be held 8 November at 9 AM EST. Register here.
Pandora Report: 10.29.2021
Laboratory testing at the CDC has identified the bacteria Burkholderia pseudomallei in an aromatherapy spray — the same type of bacteria that sickened four people in the United States earlier this year. The authors of a new article in Travel Medicine and Infectious Disease hypothesized that agents pre-occupied with espionage and counterterrorism may, at their peril, fail to correctly prioritize travel medicine. The COVID-19 pandemic has shown that false or misleading health-related information can dangerously undermine the response to a public health crisis.
No Time to Die: An In-Depth Analysis of James Bond’s Exposure to Infectious Agents
Global travelers, whether tourists or secret agents, are exposed to a smorgasbord of infectious agents. The authors of a new article in Travel Medicine and Infectious Disease hypothesized that agents pre-occupied with espionage and counterterrorism may, at their peril, fail to correctly prioritize travel medicine. To examine our hypothesis, the authors examined adherence to international travel advice during the 86 international journeys that James Bond was observed to undertake in feature films spanning 1962–2021. Scrutinizing these missions involved ∼3113 minutes of evening hours per author that could easily have been spent on more pressing societal issues. They uncovered above-average sexual activity, often without sufficient time for an exchange of sexual history, with a remarkably high mortality among Bond’s sexual partners. Given how inopportune a bout of diarrhea would be in the midst of world-saving action, it is striking that Bond is seen washing his hands on only two occasions, despite numerous exposures to foodborne pathogens. They hypothesize that his foolhardy courage, sometimes purposefully eliciting life-threatening situations, might even be a consequence of Toxoplasmosis. Bond’s approach to vector-borne diseases and neglected tropical diseases is erratic, sometimes following travel advice to the letter, but more often dwelling on the side of complete ignorance. Given the limited time Bond receives to prepare for missions, the authors urgently ask his employer MI6 to take its responsibility seriously. We only live once. Read the article here.
Twenty Years After the Patriot Act, What Is the Future of Biosecurity?
Dr. Yong-Bee Lim, recent graduate of the Biodefense PhD Program, co-authored an article – “Twenty Years After the Patriot Act, What Is the Future of Biosecurity?” – in Issues in Science and Technology. The USA Patriot Act was signed into law exactly 20 years ago, on October 26, 2001. While the law was profoundly shaped by the back-to-back events of the September 11 attacks and the 2001 anthrax attacks, it was deeply rooted in in fears about bioterrorism that had been growing since the 1990s. This anniversary provides a moment to reflect upon the Patriot Act’s legacy, as well as to imagine and plan for different biosecurity futures. The overall intent of the USA Patriot Act was clear: to prevent terrorism by raising the “barrier to entry” for potential terrorists. On its twenty-year anniversary, it is time to reflect: How well did this legislation promote or hinder biosecurity over time? In its attempts to control insider bioterror attacks, however, the implementation of the Patriot Act has triggered a series of unintended negative consequences on the life sciences, greatly disrupting who participates in science, where science is done, and how it is conducted. It is time to seriously consider whether the nation should continue these biosecurity programs as they stand today. As a diverse team of biosafety and biosecurity practitioners, the authors intend their reflections on the Patriot Act as a call to action to consider, plan, and prepare to address ongoing and emergent risks from the life sciences and biotechnology. Read the article here.
CDC Identifies Rare Bacteria in Aromatherapy Product
Laboratory testing at the US Centers for Disease Control and Prevention (CDC) has identified the bacteria Burkholderia pseudomallei in an aromatherapy spray — the same type of bacteria that sickened four people in the United States earlier this year. The spray, “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones,” was found 6 October 2021 in the home of a Georgia resident who became ill with melioidosis in late July. Melioidosis is a rare but serious disease in the United States, and it causes a wide range of symptoms that can be confused with other common illnesses, like flu or a cold. CDC is continuing testing to see if the genetic fingerprint of the bacteria in the bottle matches those of the bacteria identified in the four patients – one each in Georgia, Kansas, Texas, and Minnesota. Two of the four patients died.
The contaminated spray was sold at about 55 Walmart stores and on Walmart’s website between February and October 21 of this year when Walmart pulled remaining bottles of this spray and related products from store shelves and its website. The Consumer Product Safety Commission and Walmart are issuing a recall for the lavender and chamomile room spray and five other scents in the same product line. Investigation continues into whether other related scents and brands may pose a risk. For more information on this contaminated product, click here.
Analysis of the First Genetic Engineering Attribution Challenge
The ability to identify the designer of engineered biological sequences — termed genetic engineering attribution (GEA) — would help ensure due credit for biotechnological innovation, while holding designers accountable to the communities they affect. In a new article, the authors present the results of the first Genetic Engineering Attribution Challenge, a public data-science competition to advance GEA. Top-scoring teams dramatically outperformed previous models at identifying the true lab-of-origin of engineered sequences, including an increase in top-1 and top-10 accuracy of 10 percentage points. A simple ensemble of prizewinning models further increased performance. New metrics, designed to assess a model’s ability to confidently exclude candidate labs, also showed major improvements, especially for the ensemble. Most winning teams adopted CNN-based machine-learning approaches; however, one team achieved very high accuracy with an extremely fast neural-network-free approach. Future work, including future competitions, should further explore a wide diversity of approaches for bringing GEA technology into practical use. Read the full analysis here.
Emerging Technologies and Dual-Use Concerns: A Horizon Scan for Global Public Health
Advances in the life sciences and technology are making vital contributions to improving global health. New scientific insights that are subsequently translated into technology and refined, adapted and assimilated by innovative processes play a crucial role in advancing knowledge and addressing critical societal challenges. Yet, transformative developments in a wide range of fields can also pose risks to global health. It is therefore prudent to assess the potential adverse consequences of choosing particular technological pathways and potentially deleterious applications of technologies. Dual-use research of concern (DURC) is defined as life science research that is intended for benefit but which might be misapplied to do harm. A new report from the World Health Organization (WHO) shares the results of an international horizon scanning exercise, organized by WHO to ensure foresight. The group of experts, from a range of disciplines, undertook a broad examination of scientific and technological developments that could give rise to concern over the next two decades and identified 15 priorities. This initiative includes development of a Global Guidance Framework to Harness the Responsible Use of the Life Sciences. Biodefense program director Dr. Gregory Koblentz serves on the WHO’s advisory board of independent, international experts that are contributing to the development of this framework. Read the report here.
WHO activities on the Responsible Use of the Life Sciences intend to increase awareness and provide tools to foster benefits and constrain risks stemming from dual use life sciences and technologies. Using its role as a leader in public health globally, WHO works with Member States and relevant stakeholders to harness responsible science and to establish mechanisms for adopting changes in practice that support safe, secure and responsible life sciences. WHO strives to remain abreast of the latest developments in relevant areas of research, science, and technology to proactively identify, anticipate, and prepare for issues that hold great potential for global health. Foresight is a set of tools and techniques that help Member States and stakeholders to better prepare for a changing world, to accelerate and fully harness the gains from emerging technologies and innovation while monitoring the risks and challenges that might arise from those technologies. This is for an informed decision-making and appropriate development of strategies and frameworks for oversight and governance. Watch the WHO videos on responsible use in the life sciences and foresight here and here.
Project Aimed at Improving Safety in Labs Dealing with Lethal Viruses Receives Major Funding Grant
A project aimed at improving biosafety and biosecurity practices in high-risk laboratories working on dangerous pathogens will be led by Dr. Filippa Lentzos, Co-Director of the Centre for Science and Security Studies (CSSS) in the Department of War Studies at King’s College London, and Dr. Gregory Koblentz from George Mason University. The pair received funding to develop the Mapping Global Bio Labs project, an online tool that tracks the number of high biocontainment laboratories around the world. Also known as biosafety-level (BSL) 4 labs, these laboratories undertake hazardous research into lethal viruses to improve our understanding of diseases such as Ebola and Lassa Fever and to better prepare the world against new and emerging diseases. Research into pathogens is vital for public health, biomedical advances and disease prevention. However, these activities pose significant risks. Surges in the number of labs and an expansion in the high-risk research carried out within them have exacerbated safety and security risks. The debate on the origins of the COVID-19 pandemic has focused attention on lab leaks and safety lapses in the course of scientific research. Whether or not the pandemic resulted from an accident, the key concern is it could have. The funding will create an improved, expanded, and much more detailed resource with which to monitor these high-risk labs worldwide. It is hoped the tool will enable international organizations such as the WHO to keep a closer eye on the activities undertaken in these labs and to ensure adequate biosafety and biosecurity measures are put in place.
TECHNOLOGY
Counterintelligence Head Narrows Focus to Five Technologies Critical to US Dominance
The top counterintelligence official of the US announced that he is “narrowing his team’s to safeguarding five key technologies, including semiconductors and biotechnology, seeing their protection from rivals as determining whether America remains the world’s leading superpower.” Michael Orlando is the acting director of the National Counterintelligence and Security Center (NCSC). The NCSC is “sharpening its priorities in order to conduct an effective outreach campaign to educate businesses and academia about the expansive efforts by China and Russia to collect cutting-edge research.” The NCSC also named Edward You, a career FBI agent and expert on biothreats, to a newly created position to focus on emerging and disruptive technologies. You said that a goal in his new role is to “raise awareness that China’s efforts to develop the world’s largest data set of genetic and other biological information pose a threat beyond individual privacy issues.”
Protecting Critical and Emerging US Technologies from Foreign Threats
Given the unique opportunities and challenges posed by emerging technologies, the National Counterintelligence and Security Center (NCSC) recently announced it is prioritizing its industry outreach efforts in a select few US technology sectors where the stakes are potentially greatest for US economic and national security. These sectors produce technologies that may determine whether America remains the world’s leading superpower or is eclipsed by strategic competitors in the next few years. These sectors include, but are not limited to: artificial intelligence, bioeconomy, autonomous systems, quantum, and semiconductors.
US leadership in emerging technology sectors faces growing challenges from strategic competitors who recognize the economic and military benefits of these technologies and have enacted comprehensive national strategies to achieve leadership in these areas. The People’s Republic of China (PRC) ranks as the primary strategic competitor to the United States because it has a well-resourced and comprehensive strategy to acquire and use technology to advance its national goals, including technology transfers and intelligence gathering through its Military-Civil Fusion Policy and a National Intelligence Law requiring all Chinese entities to share technology and information with the PRC military, intelligence, and security services. Russia views the development of advanced science and technology as a national security priority and is targeting US advances through the employment of a variety of licit and illicit technology transfer mechanisms to support national-level efforts, including its military and intelligence programs.
Basic steps that individuals can take to mitigate counterintelligence risks include: using multifactor authentication; reviewing social media settings to limit the amount of your information available to the public; and never leaving electronic devices unattended while abroad. Basic steps that organizations can take to mitigate counterintelligence risks include: carefully scrutinizing the security practices of suppliers, partners, and investors; strengthening cybersecurity and hygiene; and implementing insider threat programs.
ALL THINGS COVID-19
The Impact of COVID-19 on Health and Care Workers: A Closer Look at Deaths
A new report from the World Health Organization (WHO) Health Workforce Department published a work paper that examines the impact of COVID-19 on health and care workers (HCWs), and estimates the global numbers of deaths due to COVID-19. Between January 2020 and May 2021, surveillance data reported to WHO showed 3.45 million deaths due to COVID-19. Of these only 6643 deaths were identified as being of HCWs, but this figure significantly under-reports the burden of mortality world-wide in this group. Based on the International Labour Organization’s estimated number of 135 million HCWs employed in human health and social activities and WHO’s surveillance data on all deaths reported to be due to COVID-19, mixed analytical approaches present a range between 80,000 to 180,000 deaths globally with a central population-based estimate of 115,500 deaths. In view of the mounting evidence that the number of deaths due to COVID-19 among HCWs is much greater than officially reported, the need for protection through vaccination cannot be overstated. In countries where vaccination rates of HCWs remain low, tailored communication strategies must be designed and actively pursued to increase uptake and avert vaccination hesitancy. Read the report here.
China-Linked Disinformation Campaign Blames COVID on Maine Lobsters
Marcel Schliebs is a disinformation researcher at the University of Oxford, and he tracked messaging spread on Twitter by Chinese diplomats and state media for 18 months. Schliebs discovered the emergence of a surprising (and unfounded) coronavirus origin theory: COVID-19 could have been imported to China via a batch of Maine lobsters from the US. Zha Liyou, the Chinese consul general in Kolkata, India, tweeted this claim, asserting that the lobsters were delivered to a seafood market in Wuhan, China, the city where SARS-CoV-2 first appeared. This Maine lobster theory is just the latest in a series of claims pushed by pro-China accounts since the pandemic hit. A spokesperson for the Chinese Embassy in the UK stated that China was “opposed to the fabrication and spread of disinformation.” Further, “China is the biggest victim of disinformation, and the perpetrators are some politicians and media outlets eager for China-bashing in the US and a few other Western countries.”
COVID-19 Vaccine Misinformation and Disinformation Costs an Estimated $50 to $300 Million Each Day
The COVID-19 pandemic has shown that false or misleading health-related information can dangerously undermine the response to a public health crisis. These messages include the inadvertent spread of erroneous information (misinformation) or deliberately created and propagated false or misleading information (disinformation). Misinformation and disinformation have contributed to reduced trust in medical professionals and public health responders, increased belief in false medical cures, politicized public health countermeasures aimed at curbing transmission of the disease, and increased loss of life. As a country, we do not yet have a trusted set of approaches for managing misinformation and disinformation or exact methods for monetizing the costs resulting from their spread. The challenge to assigning an exact, high-confidence monetary cost to them is the lack of detailed data available on this issue. To begin to fill this gap, the Center for Health Security developed an initial conservative estimate of the total monetized costs of one facet of this issue—the misinformation or disinformation-informed decision to not get a COVID-19 vaccine. The total COVID-19 non-vaccination has caused at least $1 billion of harm each day in the United States since vaccines became widely available. Misinformation and disinformation have caused between $50 and $300 million worth of total harm every day since May 2021. A public health effort that reduced or effectively countered misinformation and disinformation and was able to reduce related non-vaccination by 10% would be worth between $5 and $30 million per day, or between $150 and $900 million per month, while the pandemic continues.
The World Was Woefully Unprepared for a Pandemic. Let’s Be Ready for the Next One.
Just three months before the COVID-19 pandemic began, the Global Preparedness Monitoring Board (GPMB) issued a working to the international community that a pandemic was on the horizon and the world was unprepared. Their expectation came to fruition with COVID-19. Now, 20 months into the pandemic that has killed nearly 5 million people and devastated the global economy, the world remains unprepared, both to end this pandemic quickly and prevent the next one. The pandemic has exposed a “broken world of haves and have-nots where access to vaccines, treatments and PPE depends on your ability to pay.” The lack of global equity in vaccine distribution is partially a result of the “fundamental misunderstanding of global solidarity as being founded on generosity, not justice. It is also caused by longstanding systemic inequities in the global health emergency and broader international system.” Despite its many challenges, the pandemic has offered an opportunity “to celebrate the life-saving and inspiring role that science can play in mitigating dangerous diseases.” In its new report, the GPMD calls for “stronger political leadership and accountability to change the way the international community prepares for future health emergencies.” Specific recommended actions include: countries working together with civil society, the private sector and other stakeholders to take urgent steps to strengthen the ecosystem of pandemic preparedness and response; negotiating an international agreement in WHO; creating a new financing instrument at the World Bank; developing end-to-end mechanisms to advance public goods for health emergencies and share data; and empowering the WHO with strengthened with resources and authority.
Brazilian Senate Report Accuses President Bolsonaro of Crimes Against Humanity for Mishandling of COVID-19 Pandemic Response
This week, a Brazilian Senate committee approved a 1,100-page report that describes “what happens when a country’s president adopts policies with utter disregard for human rights during a pandemic.” The report portrays Brazilian President Bolsonaro as a leader who “turned his back on science and endangered the health and lives of Brazilians.” SARS-CoV-2 has thus far killed more than 600,000 Brazilians, thousands of which could have been avoided. Bolsonaro refused to follow the public health recommendations of the World Health Organization, and tried to block Congress from following those guidelines. In July 2020, he vetoed legal provisions that would have made mask wearing mandatory in churches and in the country’s overcrowded prisons. When a critical oxygen shortage emerged in Amazonas state, the Bolsonaro administration instead sent inefficacious drugs and dozens of COVID-19 patients died. The same unproven drugs were sent to Indigenous people. The report recommended a cornucopia of criminal charges against the president and called for his impeachment. In a seven-to-four vote this week, a Brazilian Senate committee recommended that Bolsonaro face a series of criminal indictments for actions and omissions related to the nation’s COVID-19 death toll, which is the second highest in the world.
From Worlds Apart to a World Prepared: GPMB 2021 Annual Report
This month, the Global Preparedness Monitoring Board (GPMB) published its third annual report, From Worlds Apart to a World Prepared. The report argues that the failures of the COVID-19 pandemic were rooted in inequality and inaction and exacerbated by geopolitical division. The Board calls for a renewed global social contract and lays out six solutions for a safer world.
The COVID-19 pandemic has exposed a world that is unequal, divided, and unaccountable. The health emergency ecosystem reflects this broken world. It is not fit for purpose and needs major reform. Hundreds of expert recommendations have been made over the last two decades, new structures have been created, but the level of ambition and action has failed to match the global need. We know what to do. We just cannot seem to do it. The current pandemic has made us more aware of the urgent need for fundamental change. There is now momentum, but new governance and funding mechanisms are being discussed behind closed doors and in limited forums. Effective transformation requires cohesive, coherent, and collaborative action. We need a new global social contract to prevent and mitigate health emergencies. The new social contract must serve as the foundation of the global health emergency ecosystem. It should be based on the principles of equity, solidarity, inclusivity and reciprocity, accountability and transparency, sustainability and action. To move from words to action, the GPMB calls for immediate action on the six most critical solutions for reform. They are:
- Strengthen global governance; adopt an international agreement on health emergency preparedness and response, and convene a Summit of Heads of State and Government, together with other stakeholders, on health emergency preparedness and response.
- Build a strong WHO with greater resources, authority, and accountability.
- Create an agile health emergency system that can deliver on equity through better information sharing and an end-to-end mechanism for research, development and equitable access to common goods.
- Establish a collective financing mechanism for preparedness to ensure more sustainable, predictable, flexible, and scalable financing.
- Empower communities and ensure engagement of civil society and the private sector.
- Strengthen independent monitoring and mutual accountability.
Read the GPMB’s report here.
EVENTS
Schar School Open House
The Schar School will be a hosting virtual open house for the Master’s and Certificate Programs! These sessions will take place on 16 November at 6:30 PM EST. This online session will provide an overview of our master’s degree programs – such as the Biodefense Program – and our Graduate Admissions team will be available to answer questions about admissions requirements, application deadlines, and materials to prepare. By working closely with faculty who draw on world-class research and practical experience, the Schar School prepares students for a high-powered career in the public, private, and non-profit sectors. Register here.
2021 Global Conference on Health and Climate Change
The 2021 Global Conference on Health & Climate Change with a special focus on Climate Justice and the Healthy and Green Recovery from COVID-19 will convene at the margin of the COP26 UN climate change conference. The aim of the conference is to call on governments, businesses, institutions and financial actors to drive a green, healthy and resilient recovery from COVID-19. The Conference will support and highlight climate action recommendations that promote and protect health. It will also mobilize the rapidly growing movement of health professionals around the world who are now driving ambitious climate action. And it will generate cross-sectoral dialogue focused on integrated solutions for a green, just and healthy future. The conference has a fully developed hybrid program, with participation both online, and in-person at the Glasgow Caledonian University. Register here.
Biorisk Management Perspective: Then and Now Webinar
In partnership with the American Biological Safety Association’s (ABSA) Biosafety and Biosecurity Month, APHL is proud to provide this free webinar! This program will provide attendees with an overview of biorisk management innovation throughout the years. Participants will hear from three biosafety professionals on their perspectives of biosafety and biosecurity practices and discuss the potential role of biosafety professionals into the future. This program is intended for anyone who works in or supervises a public health, clinical and academic/research laboratory. These can include clinical and public health laboratory staff, microbiology students, veterinary microbiology laboratory workers, veterinarians, medical doctors, biosafety professionals, academia or biotech industry laboratory workers and research scientists. The webinar will be held on 1 and 8 November from 11:30 AM to 4 PM EST. Register here.
Preparing for the Next Pandemic
The term “post-pandemic world” has become ubiquitous ever since COVID vaccines were made widely available to the developed world. Yet, the bio-policy implications of a world coming out of the COVID-19 pandemic are rarely evaluated critically and holistically. COVID-19 pandemic points to the reality that a multifaceted approach is necessary to prevent future pandemics or, should the need arise again, how to stop them in their tracks. A webinar offered by CDRF Global brings together experts from different corners of the biosafety and biosecurity space to discuss lessons learned from the world’s response to COVID-19 and analyze policy pathways moving forward. This panel will be held on 8 November at 9 AM EST. Register here.