This week’s Pandora Report covers updates from ARPA-H, new UK guidance for use of nucleic acid synthesis technologies, the UK’s recently-announced sanctions on Russian troops and organizations for use of CW in Ukraine, and more.
Upcoming Virtual Information Sessions on the Biodefense Graduate Program
If you are interested in a career in biodefense or global health security or want to develop the knowledge and skills necessary to work at the nexus of health, science, and security, find out what the Schar School of Policy and Government has to offer.
A virtual open house for the MS in Biodefense will be held online on Thursday, October 17, 7 to 8 p.m. ET . The Biodefense Program offers flexible part-time or full-time options that teach applicable, real-world skills for bridging the gap between science and policy. The online session will provide an overview of the program, as well as the application process, student experience and graduate outcomes. Register here.
The Schar School PhD programs will be holding a virtual open house on Wednesday, October 30 from 6-7:30 PM. Please join Dr. Gregory Koblentz, director of the Biodefense Graduate Program, to learn more about the Biodefense PhD program and ask any questions you may have. Register here.
ARPA-H Launches Predictive Drug Safety and Efficacy Model Program
The Advanced Research Projects Agency for Health (ARPA-H), part of the Department of Health and Human Services, recently announced a new funding opportunity through its Computational ADME-Tox and Physiology Analysis for Safer Therapeutics (CATALYST) program. The program aims to create human physiology-based computer models to accurately predict safety and efficacy profiles for Investigational New Drug (IND) candidates.
The announcement explains “Through a forthcoming Innovative Solutions Opening (ISO) solicitation, CATALYST invites proposals across three technical areas: data discovery and deep learning methods for drug safety models, living systems tools for model development, and in silico models of human physiology. If successful, CATALYST will significantly improve drug safety testing in preclinical and clinical studies and create a drug development tools pipeline for use in regulatory science applications.”
Read more here.
UK Announces Sanctions on Russian Troops Using CW in Ukraine
The UK government announced this week that it has sanctioned Radiological, Chemical and Biological Defence Troops of the Russian Armed Forces and their leader, Igor Kirillov, following their use of chemical weapons in Ukraine. The announcement also described Kirillov as “a significant mouthpiece for Kremlin disinformation, spreading lies to mask Russia’s shameful and dangerous behaviour.” The UK also sanctioned two Russian MOD laboratories (the 27th Scientific Centre and the 33rd Central Scientific Research and Testing Institute) for the support they provided in developing and deploying the weapons.
UK Publishes Voluntary Guidance for Providers and Users of Synthetic Nucleic Acid
“The UK National Vision for Engineering Biology, published in December 2023, set out an ambition for the UK to be a world leader in responsible innovation in engineering biology. This Guidance delivers on that ambition by championing and enabling the legitimate use of nucleic acid synthesis technologies, whilst reducing the risks which could result from accidental or purposeful misuse.”
“The Guidance makes recommendations to UK providers and users of synthetic nucleic acid to promote screening practices. It supports the safe study or engineering of existing or novel biological systems to help unlock the exciting benefits of this technology in applications across healthcare, chemical and materials, low carbon fuels, and agriculture. Uptake of the Guidance will be reviewed to ensure that it is providing proportionate guardrails.”
Read Christopher East’s discussion of this guidance in this piece from the Council on Strategic Risks-“New “Gene Synthesis Screening Guidance” in the UK: A Positive Step Towards Responsible Innovation”
UK Department for Science, Innovation and Technology Launches Regulation Innovation Office
The UK government also recently announced the creation of the Regulation Innovation Office, which aims to “reduce the burden of red tape and speed up access to new technologies that improve our daily lives – from AI in healthcare to emergency delivery drones”. The announcement explains that “The new Regulatory Innovation Office (RIO) will reduce the burden for businesses hoping to bring new products and services to the market in some of the UK’s fastest-growing sectors through innovations like –AI training software for surgeons to deliver more accurate surgical treatments for patients and drones which can improve business efficiency and quickly send critical deliveries to remote parts of the country.”
“To do so, it will support regulators to update regulation, speeding up approvals, and ensuring different regulatory bodies work together smoothly. It will work to continuously inform the government of regulatory barriers to innovation, set priorities for regulators which align with the government’s broader ambitions and support regulators to develop the capability they need to meet them and grow the economy.”

“National Security Debate on Global Health Enters a New Phase”
David P. Fidler discusses the debate about the expansion of the concept of national security and how global health fits into this in this piece for Think Global Health: “To date, the securitization of pandemics and climate change in U.S. policy has become orthodoxy but has failed, which raises questions about the value of national security arguments concerning global health problems. Geopolitical competition and polarized domestic politics are shrinking what national security means in U.S. policy, making national security claims about global health threats even more difficult to sustain.”
“Pathway to a Healthier America: A Blueprint for Strengthening Public Health for the Next Administration and Congress”
This report from Trust for America’s Health “…provides the Administration and Congress taking office in 2025 a policy roadmap for improving the nation’s health, economy, and national security.” It outlines several priorities, such as investing in public health infrastructure and workforce, improving health security threat readiness, and promoting health across the lifespan.
“Optimizing Federal, State, and Local Responses to Public Health Emergencies: Lessons from COVID Proceedings of a Workshop—in Brief”
From NASEM: The National Academies of Sciences, Engineering, and Medicine’s Committee on Science, Technology, and Law is pleased to announce the release of the proceedings of its May 30-31, 2024 workshop, Optimizing Federal, State, and Local Response to Public Health Emergencies. The workshop, which was organized by a planning committee co-chaired by Georges Benjamin (American Public Health Association) and Erwin Chemerinsky (University of California, Berkeley School of Law), featured the following sessions: Optimizing Federal, State, and Local Public Health Preparedness, The COVID-19 Pandemic: What happened? What went right? What went wrong? –, Public Health Emergency Authorities: What we know about them and how did we experience them before, during, and after the COVID-19 pandemic?, Exploring Routes and Barriers to Effective Public Health Response Efforts During the COVID-19 Pandemic, Looking to the Future: Where do we go from here?, and Concluding Thoughts from Workshop Planning Committee.
“AI in Public Health: Gaps, Disparities, and Remarkable Potential”
Shi En Kim covers a panel-“Making AI a Lifesaver”-hosted by the Johns Hopkins University Bloomberg Center in Washington DC in this article for Global Health Now, writing in part “The panelists broadly agreed that there needs to be more transparency in how AI is being used. For starters, noted Ehrenfeld, better visibility into AI will help flag flaws that lead to inequity as well as make AI a more effective tool for public health workers. Stuart noted the clear need for training on AI’s ethical issues and applications presents a big opportunity for schools of public health and medical schools.”
“Framework for Nucleic Acid Synthesis Screening”
The NSTC’s Fast Track Action Committee on Synthetic Nucleic Acid Procurement Screening recently released this framework: “This framework outlines a unified process for screening purchases of synthetic nucleic acids and benchtop nucleic acid synthesis equipment. While the framework will be incorporated into requirements for recipients of federal research funding, including through domestic and international funding documents, broader use of the framework is encouraged. This approach guides providers of synthetic nucleic acids (“Providers”) and manufacturers of benchtop nucleic acid synthesis equipment (“Manufacturers”) to screen purchase orders to identify sequences of concern (SOCs) and assess customer legitimacy.”
“A New Biosecurity Strategy for the World to Follow”
CSR’s Jackson du Pont discusses CEPI’s recently launched Biosecurity Strategy in this blog post, writing in part “On Wednesday, September 25th, the Coalition for Epidemic Preparedness Innovations (CEPI) launched its inaugural Biosecurity Strategy—an incredibly important contribution towards galvanizing efforts to advance global biosecurity prioritization and governance. It represents a significant step in strengthening biosecurity norms and should serve as a model for future efforts to increase investments in addressing biological risks in the safest, most responsible ways possible.”
DHS Releases 2025 Homeland Threat Assessment
The Department of Homeland Security (DHS) recently released its Homeland Threat Assessment (HTA) for 2025. The HTA aims to “…inform both the public and the Department’s partners of the threats to public safety and security, in order to assist federal, state, and local partners in preparing, preventing, and responding to an ever-evolving threat environment.” This year’s HTA explains that the threat environment is expected to “remain high” in the coming year. Among other topics, the HTA also discusses the potential for CBRN attacks and nefarious use of emerging technologies:
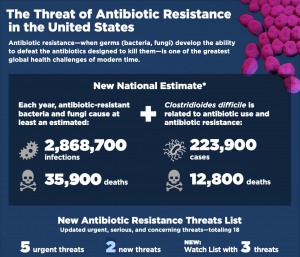
“We expect predominantly aspirational and rudimentary interest in CBRN attacks will continue in 2025. Among foreign and domestic threat actors, we assess that DVEs and criminals will remain the most likely perpetrators of deliberate CBRN-related attacks. Over the last year, there were 18 known deliberate chemical- or biological-related incidents in the Homeland, four of which were linked to political or ideological motives while the rest were criminal in nature. All of the incidents employed simple methods, and one incident caused at least one death. Two of the 18 incidents involved the alleged use of ricin, while 14 of the incidents employed easily obtainable chemicals—including a range of pesticides, chlorine, bear spray, and other chemical irritants. Fentanyl was weaponized in two instances. Foreign and domestic threat actors maintain aspirational interest in radiological and nuclear attacks, but these attacks remain unlikely.”
“We expect threat actors will continue to explore emerging and advanced technologies to aid their efforts in developing and carrying out chemical and biological attacks. Over the last year, foreign and domestic extremists online expressed interest in using DNA modification to develop biological weapons to target specific groups. We remain concerned about the potential exploitation of advances in artificial intelligence (AI) and machine learning to proliferate knowledge that supports the development of novel chemical or biological agents. (For more information on AI and threat actors, see pages 26–27.) Such advances could be exploited by state and state-sponsored adversaries, but the necessary expertise for such exploitation most likely exceeds that of most nonstate actors. We also remain concerned about the potential for threat actors to use unmanned aircraft systems (UAS) in chemical or biological attacks due to the continued advancement of UAS technology and the growing availability of UAS.”
“Tehran’s Tactical Knockout: Weaponized Pharmaceutical-Based Agents”
Matthew Levitt discusses Iran’s use of PBAs in this article from the CTC Sentinel: “As early as the 1980s, the U.S. intelligence community documented the ways in which Iran deployed chemical weapons for tactical delivery on the battlefield. Nearly 40 years later, U.S. officials formally assessed that Iran was in non-compliance with its Chemical Weapons Convention (CWC) obligations, pointing specifically to Tehran’s development of pharmaceutical-based agents (PBAs) that attack a person’s central nervous system as part of a chemical weapons program. Over time, concern about this program has increased, with reports to the Organisation for the Prevention of Chemical Weapons (OPCW), statements by multilateral groups such as the G7, and a variety of U.S. government reports and sanctions. Today, with Iran’s proxies wreaking havoc throughout the region, officials worry Tehran may have already provided weaponized PBAs to several of its partners and proxies. Such a capability, tactically deployed on the battlefield, could enable further October 7-style cross-border raids or kidnapping operations. With the region on edge following the targeted killing of Hezbollah leader Hassan Nasrallah, followed by an Israeli ground campaign targeting Hezbollah infrastructure along the border, and the Iranian ballistic missile attack on Israel, concern about the use of such tactical chemical weapons is high.”
What We’re Listening to 🎧
Poisons and Pestilence: ‘Back to Source’ with Seth Carus
“In this bonus episode I am joined by Seth Carus, as we explore some of the earliest allegations of biological warfare- as well as the more recent modern developments, which transformed ancient fears, into Cold War era weapon systems.”
Listen here.
NEW: The Advancing Threat Agnostic Biodefense Webinar Series
From PNNL: “Please join us in welcoming Drs. Matthew Kasper and Lindsay Morton from the Department of Defense (DoD) Global Emerging Infections Surveillance (GEIS) program for their talk titled “Challenges and Opportunities in Pathogen Agnostic Sequencing for Public Health Surveillance: Lessons Learned From the Global Emerging Infections Surveillance Program.” This webinar will take place Tuesday, October 29th, at noon PT.”
Learn more and register here.
Potential Research Priorities to Inform Readiness and Response to Highly Pathogenic Avian Influenza A (H5N1)
“The National Academies will host a 2-day virtual public workshop, October 22-23, to explore research priorities for the ongoing H5N1 outbreak in the U.S. Recognizing the interconnection between people, animals, and their shared environment, this workshop will take a One Health approach to bring together federal government agencies, the academic community, and the private sector, as well as other relevant stakeholders across the health, agriculture, and food safety sectors.”
“Workshop discussions will focus on basic science and research areas of concern and may help inform future research that could provide local, national, and global communities with information about virus transmission, mitigation of risks, and appropriate measures to prevent the spread of disease.”
Learn more and register here.
One Health and the Politics of COVID-19 Book Launch
The Writer’s Center is hosting a book launch for Dr. Laura Kahn’s new book, One Health and the Politics of COVID-19 (blurb below) on November 23 at 2 pm EST in Bethesda, MD. Learn more and RSVP here.
“One Health and the Politics of COVID-19 unpacks the mysteries of COVID-19’s origins to impart important lessons for future outbreaks. The One Health concept recognizes the interconnected links among the health of humans, animals, plants, and the environment. By comparing the history, science, and clinical presentations of three different coronaviruses—SARS-CoV-1, MERS, and SARS-CoV-2 (COVID-19)—Kahn uncovers insights with important repercussions for how to prepare and avoid future pandemics. The One Health approach provides a useful framework for examining the COVID-19 pandemic. Understanding the origins of this zoonotic disease requires investigating the environmental and molecular biological factors that allowed the virus to spread to humans. The book explores the many ways in which the wild animal trade, wet markets, and the camel industry contributed to the spread of the earlier SARS-CoV-1 and MERS coronaviruses. For SARS-CoV-2 (COVID-19), Kahn examines the biosafety, biosecurity, and bioethics implications of gain-of-function research on pandemic potential pathogens. This book is a must read to understand the geopolitics of the COVID-19 pandemic.”
NEW-US AI Safety Institute Issues RFI on Responsible Development of Chem-Bio Models
From AISI: “The U.S. Artificial Intelligence Safety Institute (U.S. AISI), housed within the U.S. Department of Commerce’s National Institute of Standards and Technology (NIST), released a Request for Information seeking insight from stakeholders regarding the responsible development and use of chemical and biological (chem-bio) AI models.”
“Input from a broad range of experts in this field will help the U.S. AISI to develop well-informed approaches to assess and mitigate the potential risks of chem-bio AI models, while enabling safe and responsible innovation.”
“Respondents are encouraged to provide concrete examples, best practices, case studies, and actionable recommendations where possible. The full RFI can be found here.”
“The comment period is now open and will close on December 3, 2024, at 11:59PM Eastern Time. Comments can be submitted online at www.regulations.gov, under docket no. 240920-0247.”
NEW-Infodemic Management Course from Open WHO
“In the recent years, the circulation of health misinformation and disinformation has exploded with the digitalized information ecosystem. They cause confusion and risk-taking behaviours that can harm health. They also lead to mistrust in health authorities and undermines the public health response. Misinformation and disinformation can intensify or lengthen outbreaks when people are unsure about what they need to do to protect their health and the health of people around them especially during health emergencies. Public health workers need knowledge and skills to manage harm from health misinformation and disinformation. This course will help them to better understand the infodemic mechanisms that underlie the emergence and spread of misinformation, the complex and harmful nature of disinformation and how to intervene to better prevent and respond to both of these types of information-based harms.”
Access this self-paced course here.
NEW-ACHS Fellowship Program 2025
From the Asia Centre for Health Security: “The ACHS Fellowship Program aims to inspire and connect the next generation of biosecurity leaders and innovators.”
“Newly launched in 2025, ACHS Fellowship is a highly competitive, part-time program that provides an opportunity for talented graduate students and professionals to deepen their expertise, expand their network, and build their leadership skills through a series of training and project work coordinated by the Asia Centre for Health Security based at the Saw Swee Hock School of Public Health, National University of Singapore (NUS).”
“This 12-month fellowship does not require relocation to Singapore and can be completed alongside full-time employment or an academic schedule.”
Learn more and apply here.
External Review of Ethical, Legal, Environmental, Safety, Security, and Societal Issues of Engineering Biology Research and Development
From NASEM: “Engineering biology holds significant potential to transform the U.S. and global economy, with promise to deliver innovative solutions in health, climate, energy, food and agriculture, and more. As research and development in engineering biology and other areas of the bioeconomy advance, addressing the societal issues related to these technologies is imperative. As requested by the CHIPS and Science Act, this study will conduct an evaluation of the ethical, legal, environmental, safety, security, and other societal issues related to engineering biology, and make recommendations on research needs related to these issues and means to effectively incorporate their consideration into research practice.”
“The National Academies of Sciences, Engineering, and Medicine (NASEM) will appoint an ad hoc committee to review and make recommendations on the ethical, legal, environmental, safety, security, and other appropriate societal issues related to engineering biology research and development. The committee will address the scholarship and practice of addressing these issues, focusing specifically on:
(1) An assessment of the current knowledge and practice on assessing and mitigating various societal issues including ethical, legal, environmental, safety, and security issues.
(2) A description of the gaps and needs relating to such issues, focusing on approaches for co-generation of assessment approaches and design of products, technologies, and services with users of engineering biology research and development
(3) Actionable recommendations on how the National Engineering Biology Research and Development Initiative, established by the CHIPS and Science Act, can address the identified gaps and needs.
(4) Actionable recommendations on how researchers across the range of disciplines engaged in engineering biology can best incorporate considerations of such societal issues into the development of research proposals and the conduct of research.”
“NASEM will produce a consensus report presenting the results of its work and offering its findings, conclusions, and recommendations.”
“We invite you to submit suggestions for experts to participate in this activity. The call for experts closes on October 16, 2024 at 11:59 (ET).”
Recommend an expert here.