By Michelle Grundahl, Biodefense MS Student
On May 26, 2021, the National Biodefense Science Board (NBSB) held a (virtual) public meeting that discussed actions that the United States needs to take to be better prepared for the challenges posed by public health emergencies such as pandemics, “Disease X,” and other biological threats. NBSB is the federal committee that advises the office of the Assistant Secretary for Preparedness and Response (ASPR) in the U.S. Department of Health and Human Services (HHS). During the meeting, the NBSB presented their recommendations to ASPR from its new report on ‘filling critical gaps’ in health emergency preparedness, response, and recovery. In addition, NBSB was briefed on the CDC’s new initiative to improve its data collection and analytical capabilities to improve information sharing and situational awareness during a public health emergency.
The NBSB’s All-Hazards Science Response Working Group draft report, Filling Critical Gaps: Comprehensive Recommendations for Public Health Preparedness, Response, and Recovery from the National Biodefense Science Board, is the result of a September 2020 request from ASPR to NBSB to review the 2007 Homeland Security Presidential Directive 21 (HSPD-21). HSPD-21 is the national strategy for ‘Public Health and Medical Preparedness’ that was formulated during the George W. Bush Administration as part of its strategy to protect the health of Americans during disasters. ASPR asked NBSB to answer three questions:
1) What, if any, of the 2007 focus areas (biosurveillance, countermeasures stockpiling and distribution, mass casualty care, or community resilience) should remain as highest priorities for capacity development by HHS?
2) How might those focus areas be modified, updated, or expanded to promote additional advances in public health and medical preparedness in the United States?
3) What should be new HHS focus areas for public health and medical preparedness, if any?
The key finding of the NBSB report is that the United States should always be prepared to “implement an immediate, effective, and coordinated public health response that is guided by scientific knowledge and protected from undue political influence…insulated from political considerations, with the ability to independently develop, directly distribute, and frequently update public health messages with scientific principles in mind, guided by analysis of available data, with inputs from the nation’s leading experts.” To achieve that objective, NBSB made five recommendations to enhance the country’s disaster preparedness and response based on strengthening One Health biosurveillance and situation awareness, enhancement of medical countermeasures, reinforcing health workforce readiness, increasing health facility resilience, and improving communication with the public during health crisis.
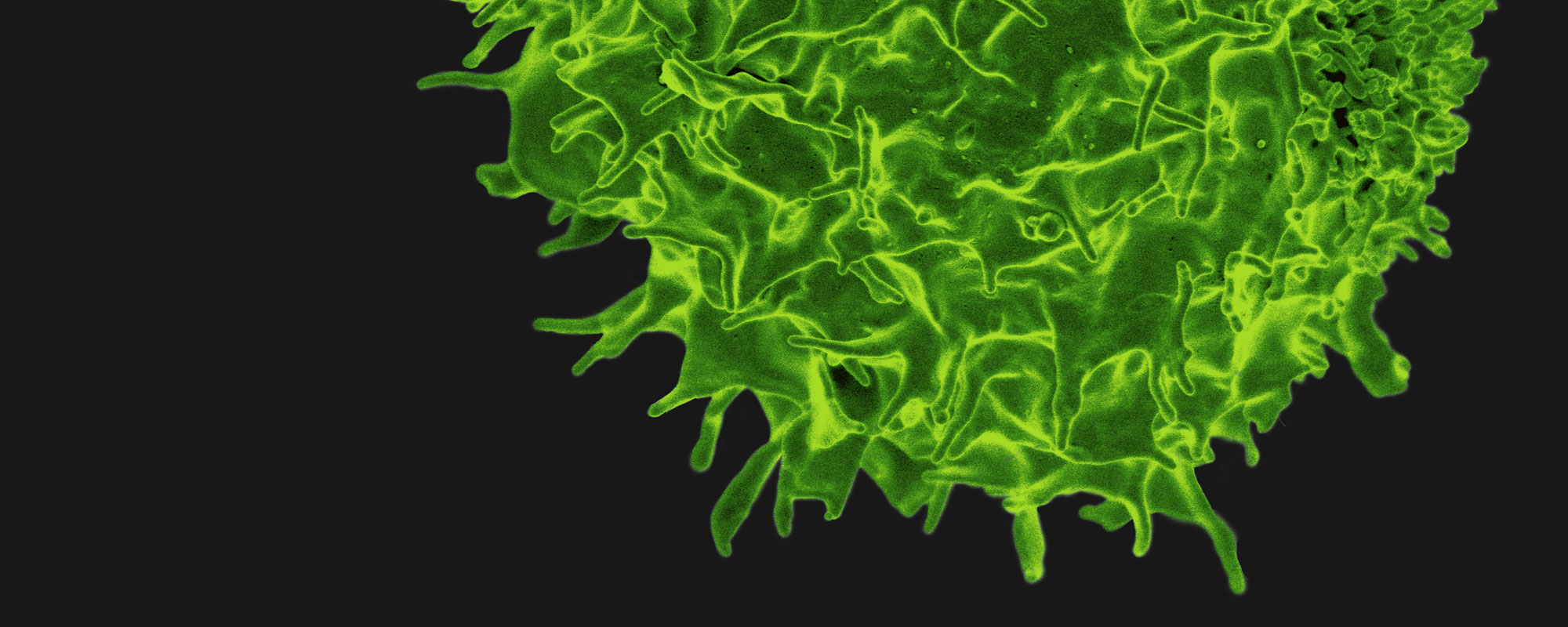
The NBSB’s first recommendation is to use a One Health threat assessment for biosurveillance and situational awareness. One Health is holistic approach that considers the systems involved in achieving optimal health outcomes for humans, animals, plants and their shared environment. NBSB recommended that federal departments, public and private research institutions, and private sector organizations should engage in One Health collaborations to protect against emerging human and animal disease risks. A One Health approach would continuously assess emerging human and animal disease risks by using research and predictive data capabilities (based on artificial intelligence) to assess patterns of animal, agricultural, and human health. Proactively discovering biothreats, including zoonotic or arthropod-borne disease, would create improved situational awareness about high consequence risks.
The board specifically suggests the enhancement of medical countermeasures (MCM), manufacturing, and supply chain. The report provides detailed examples of this approach, and advises that the production of vaccines, drugs, personal protective equipment, and diagnostics should all be “on-shored” inside the United States for quick production and scale-up. For example, active pharmaceutical ingredients, as well as finished products, can be made in the United States instead of imported from foreign suppliers. In addition, assessment of emergency medical countermeasures and diagnostic tools, as well as readiness for manufacturing them, should be an ongoing process. Also, mechanisms for infectious disease, vector-borne and zoonotic disease research and related drug development require investment in computer modeling, in-vitro models, and better animal models. To support these goals, NBSB recommend that incentives should be provided to support private sector innovation. The board also suggests improving the transparency of the Public Health Emergency Medical Countermeasures Enterprise (PHEMCE) to increase information sharing among relevant Federal agencies and private sector partners. The PHEMCE – led by ASPR – consists of coordinated federal preparedness activities and medical countermeasures for natural, accidental, and intentional threats. Federal interoperable capabilities should be ready to be deployed systematically to proactively manage zoonotic and infectious diseases, climate change, supply chain shortages, workforce shortages, and additional threats to health security.
The health workforce is another focus area for achieving readiness and resilience during a public health crisis. The nation’s workforce needs more infectious disease specialists who are the first responders during an outbreak or a pandemic. The NBSB suggested that the training curriculum for health professionals should include disaster preparedness, emergency response, epidemic control, and training to use personal protective equipment. Likewise, first responders and incident commanders would benefit from additional emergency response education related to health threats and disasters. A critical point identified by NBSB is the need to review Emergency Support Function (ESF)-8 of the National Response Framework which coordinates of public health and medical services in response to a natural disaster, terrorist attack, or other incidents of national significance. Another astute point is the consideration of the need for childcare, eldercare, and pet care to be available for health workers and first responders during disasters.
NBSB also identified health facility readiness and resilience (and the general soundness of healthcare systems) as having room for improvement as well. Some examples of improvements that are desperately needed are stronger health facility cybersecurity, better hospital collaborations for resource sharing (including staff), and planning for weather disasters overlapping with simultaneous health threats. As a lesson learned from COVID-19, telehealth and health license portability should continue post-pandemic. During COVID-19, health appointments could be held remotely online, and health professionals could work outside of their licensed jurisdictions. Since electronic health records are available over the internet, health professionals could see patients from anywhere.
The NBSB also recommended improving public communication by developing and disseminating “timely, accurate, consistent, and trusted advisories, public health messages, and clinical guidelines” during a health crisis. Clear, consistent scientific messages should not be influenced by political concerns. Their communication recommendation noted that there should be an alignment of information using social media and local organizations. The goal is to provide accurate information to everyone; no one in society should be left out of receiving crisis communications.
The recommendations contained in this report build on previous reports by NBSB on how to “accelerate research and develop goals to prevent infectious diseases disasters.” For example, the May 13, 2020 report, Medical Countermeasure Research and Development Goals to Prevent Infectious Disease Epidemics, recommended nine items for the early detection and identification of pathogens, including early activation of MCM, coordination mechanisms, rapid MCM development pathways, adequate infrastructure and emergency funding – and the management of public trust. Another May 2020 report, Integrating Clinical Disaster Response Training with Community and State-Based Emergency Planning, recommended continued collaborations between clinical practitioners and disaster management authorities. That previous report focused on medical recommendations for healthcare organizations, local health departments, incident commanders, and emergency medical services to improve their capacity for disaster response, recovery, and mitigation.
The NBSB also heard from Dr. Daniel B. Jernigan, Deputy Director for Public Health Science and Surveillance, about the Centers for Disease Control and Prevention (CDC) Data Modernization Initiative. The CDC now has greater capacity to use electronic data and centralized laboratory reporting. They can receive and share massive data through the cloud. The CDC is still aiming for an even more modern, integrated, real-time public health surveillance data. This initiative involves four core areas for strengthening core surveillance capabilities: 1) syndromic surveillance, 2) electronic case reporting (eCR), 3) electronic laboratory reporting, and 4) vital records. Syndromic surveillance can reveal local symptom trends by comparing hospital and health reports. Dr. Jernigan discussed real-time data surveillance during COVID-19, which used county-level monitoring of COVID-like Illness (CLI). Anomaly detections and syndromic surveillance programs, such as BioSense, are cloud-based. Electronic case reporting is the real-time automated information exchange of electronic health records between public health agencies. Reporting laboratory results electronically reduces the turn-around time of waiting for results, allowing for faster intervention. Electronic lab reporting existed before COVID-19, but it was not automated or truly robust. Also, having up-to-date information on vital records, such as death certificates, is important for public health decision-making.
The goal of the CDC’s data modernization plan is to collect accurate data, including from non-traditional sources that can forecast health threats, that can be shared easily with partners. Under this model, data would flow through the same data hubs, where a single data upload would inform various partners in a hub and spoke model. Faster access to larger data sets will allow for interoperability and dashboards that inform forecasting and decision-making. Combined data-set platforms can be used to create pandemic dashboards. Timely, high-quality data sharing is now scalable and the process can be used during future outbreaks to reduce the burden of manual reporting. Data standards for electronic data exchange and electronic data linkage, using databases such as the National Notifiable Diseases Surveillance System (NNDSS), will bolster the mapping of notifiable diseases.
Together, the draft report by the NBSB’s All-Hazards Science Response Working Group and the CDC’s data modernization plan can help strengthen public health emergency preparedness and response in the United States so that we can prevent pandemics – and be ready for unknown threats.