Jay Bickell is a student in the MS Biodefense program at the Schar School of Policy and Government at George Mason University. In her current position as a Staff Scientist at MRIGlobal, Jay supports biorisk management programs for various commercial, academic, and government clients.
In August 2024, three alumni of the George Mason University (GMU) Biodefense PhD program— Dr. Jomana Musmar, Dr. Yong-Bee Lim, and Dr. Saskia Popescu —could be found in the United Kingdom at the Wilton Park workshop Through the Kaleidoscope: Antimicrobial Resistance, Conflict and Security. This workshop convened leading experts to assess the growing biosecurity threats posed by antimicrobial resistance (AMR).
Wilton Park, for some background, is an Executive Agency of the UK Foreign, Commonwealth & Development Office that was established after World War II as a hub for international policy discussions. Today, it serves as a discreet space where experts come together and roll up their sleeves to address some of the most complex global challenges. For many individuals, being invited to attend a Wilton Park event can be considered one of the greatest honors and highlights of a career, and receiving an invitation is no easy feat. Attendance at Wilton Park events requires deep subject matter expertise, background checks, and a strong professional network. Housed in a beautiful 16th century mansion in the English countryside, Wilton Park looks and feels more like Downton Abbey than a traditional think tank.

The Kaleidoscope dialogue brought together approximately 40 high-level experts from the United States and the United Kingdom. The workshop report, published in March 2025, highlights that “AMR increases the risks of public health system collapse, accelerates biosecurity concerns, and heightens societal vulnerabilities.” In particular, the report underscored the growing threat of multidrug resistance to both military and civilian operations particularly in conflict zones. The presence of three GMU Biodefense alumni at such an important gathering is a testament to both their individual achievements and the strength of the GMU Biodefense program.
Dr. Jomana Musmar (PhD Biodefense, 2017)
Since earning her doctorate, Dr. Musmar has played a key role in U.S. health security policy within the Office of the Assistant Secretary for Health. She manages the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB). Established under an executive order in 2014, PACCARB provides advice and recommendations to the Secretary of Health and Human Services on programs and policies to combat antibiotic resistance in human, animal, and environmental health. Dr. Musmar recently expanded her role to Deputy Director of Strategic Initiatives, overseeing national strategies on vaccines, STIs, HIV/AIDS, and viral hepatitis. At Wilton Park, she contributed her expertise on antimicrobial resistance and emphasized how environmental and agricultural factors can act as force multipliers in the security implications of AMR.
Dr. Yong-Bee Lim (PhD Biodefense, 2021)
Since earning his doctorate Dr. Lim has been with the Council on Strategic Risks where his work has focused on the intersection of biosecurity, health security, emerging technologies, and the ways risks can converge, interact with, and exacerbate each other. However recent congratulations are in order as Dr. Lim just started a new position as an Associate Director of the Global Risks team at the Federation of American Scientists. His extensive national and international biosecurity network helped secure him a seat at the Wilton Park Kaleidoscope dialogue, where he not only contributed his expertise but also facilitated a guided discussion session and helped review the final event report. Reflecting on the experience, he emphasized that while there is a lot of work to be done to address AMR, there are actionable solutions and dedicated professionals working toward them.
Dr. Saskia Popescu (PhD Biodefense, 2019)
Earning her doctorate just before the COVID-19 pandemic began, Dr. Popescu’s expertise in clinical infection prevention and biodefense landed her in a role developing a hospital bio-preparedness program. She then transitioned to an infection prevention role at Netflix, supporting continuity of operations during a global health crisis. She currently works as a policy researcher for RAND while also serving as an adjunct professor at GMU and an assistant professor at the University of Maryland. Her unique blend of infection prevention, AMR, and biosecurity expertise made her an invaluable contributor at Wilton Park, where she provided a frontline public health perspective. Dr. Popescu also helped review the final event report, and her briefing, AMR and Public Health, is featured in the report’s expert contributions section.
A Kaleidoscope of Perspectives
At the Wilton Park AMR event, these three exceptional GMU alumni engaged with experts across diverse fields including philosophy, national security, veterinary medicine, cultural anthropology, and synthetic biology. A common reflection from all three alumni was the remarkable collaboration and kindness among attendees — a sentiment that clearly extends to Dr. Musmar, Dr. Lim, and Dr. Popescu themselves. Interestingly, the final Kaleidoscope report does not explicitly define the connection between its title and AMR, leaving room for interpretation. In a kaleidoscope, mirrors angled towards each other reflect objects within them, creating shifting patterns. Two people will never see the exact same pattern in a kaleidoscope because of slight differences in their viewing angles and the way the mirrors and objects are arranged. Similarly, AMR is an evolving challenge, with new complexities and solutions emerging as it is examined from the perspectives of different disciplines. The diverse expertise of Dr. Musmar, Dr. Lim, and Dr. Popescu, spanning policy, biosecurity, public health, and more, reflects the creativity needed to tackle AMR, and how interdisciplinary collaboration is shaping the evolving landscape of health security.
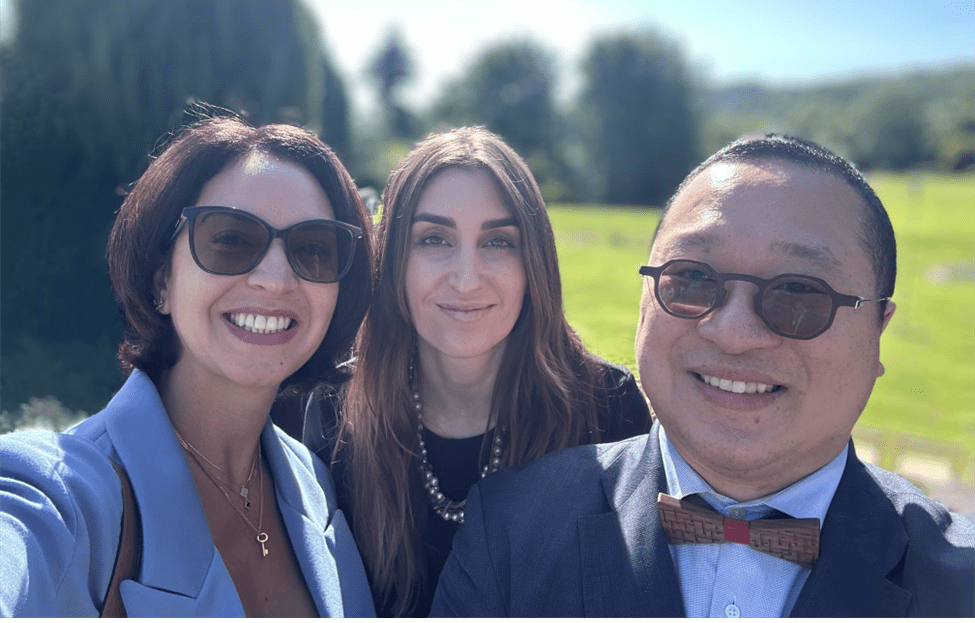
Left to right: Dr. Jomana Musmar, Dr. Saskia Popescu, and Dr. Yong-Bee Lim at Wilton Park