Highlights include a new Q-fever vaccine, MERS in Qatari camels, revised 2009 H1N1 deaths, black silicon the bacteria slayer, and the new, FDA-approved, H5N1 vaccine. Happy Friday!
Eyeing Terrorist Potential, Pentagon Seeks Vaccine Against Cold War-Era Bioweapon
The Pentagon is pushing forward with plans to develop a vaccine against Q-fever, the disease caused by the bacterial agent Coxiella burnetii. While the majority of Q-fever cases are asymptomatic, C.burnetti is a spore former, and is therefore both hardy and stable. However, as the primary reservoirs of the disease are sheep, goats and cattle, the disease tends to be confined within slaughterhouse workers. The acute form of the disease has a fatality rate of less than one percent, while the chronic form ranges from five to 25%.
National Journal – “The United States investigated the agent’s warfare potential and the Soviet Union fully weaponized it decades ago, long before both countries formally denounced biological arms in the 1970s. The disease also occurs in nature and has affected hundreds of U.S. troops deployed overseas. It can produce fever, pneumonia, and numerous other symptoms associated with a variety of pathogens. Certain antibiotics are considered effective against the bacteria, but no vaccine is presently sold in the United States, according to the Federation of American Scientists. An existing vaccination available abroad reportedly can cause side effects such as abscesses and swollen joints.”
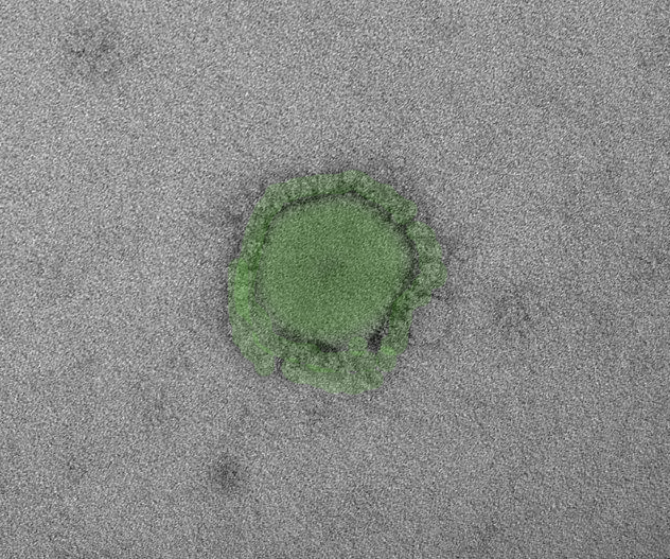
MERS virus found in camels in Qatar, linked to human spread
The Middle Eastern Respiratory virus has been detected in three Qatari camels, according to an unpublished study. While the press release does not detail whether live virus or antibodies to the virus were detected, there have been two confirmed cases of human infection related to the barn housing the infected camels. Although camels and bats are the leading candidates for potential reservoirs of the virus, there still exists too little conclusive evidence supporting either.
Reuters – “British researchers who conducted some of the very first genetic analyses on MERS last September said the virus, which is from the same family as Severe Acute Respiratory Syndrome, or SARS, was also related to a virus found in bats…Ab Osterhaus, a professor of virology at the Erasmus Medical Centre in The Netherlands that worked on the camel study, told Reuters the results were confirmed by a range of tests including sequencing and antibody testing. Dutch scientists said in August they had found strong evidence that the MERS virus is widespread among one-humped dromedary camels in the Middle East – suggesting people who become infected may be catching it from camels used for meat, milk, transport and racing.”
W.H.O. Estimate of Swine Flu Deaths in 2009 Rises Sharply
The WHO has significantly revised its fatality estimates for the 2009 outbreak of H1N1, which are estimated be ten times too low. It’s original numbers were just over 18,000 – according to a study published this week, the number of fatalities from the virus alone was actually closer to 203,000. When fatalities resulting from secondary conditions because of the virus are counted, the number approaches 400,000. There are a couple of important reasons for revising fatality counts, the first of which is it remedies accusations of sensationalizing the potential threat to sell vaccines.
New York Times – “The estimated death toll closely matches that of a study published in June 2012 by the Centers for Disease Control and Prevention. That study, based on early data, estimated that 201,000 people died of flu and respiratory causes and another 83,000 died of related cardiac problems. Both counts were many more than the 18,449 laboratory-confirmed cases that the W.H.O. stood by as its official count in 2009 because agency officials were reluctant to guess at fatality rates. Some politicians, particularly in Europe, used the low official W.H.O. death rate to argue that fear of the pandemic had been overblown. They accused vaccine companies of fanning the public’s fears to sell more of their product.”
Bactericidal activity of black silicon
From dragonfly’s wings to black silicon? In a recent study originating from Australia, scientists discovered that dragonfly wings were absolute shredders of bacteria. The structure of the wings destroys bacterial cell walls of both gram positive and gram negative bacteria upon contact. Now, shown that black silicon has similar bactericidal properties as well. While black silicon is not readily mass produced, there are several substances with similar nano features which can be. Our first thoughts here are hospitals and doorknobs.
Nature – “Both surfaces are highly bactericidal against all tested Gram-negative and Gram-positive bacteria, and endospores, and exhibit estimated average killing rates of up to ~450,000 cells min−1 cm−2. This represents the first reported physical bactericidal activity of black silicon or indeed for any hydrophilic surface. This biomimetic analogue represents an excellent prospect for the development of a new generation of mechano-responsive, antibacterial nanomaterials.”
FDA approves H5N1 bird flu vaccine
The FDA has approved the first adjuvanted H5N1 vaccine, designed primarily for those who have frequent interactions with poultry. As the vaccine is adjuvanted, less antigen is required to stimulate an immune response. The vaccine, which is administered in two doses three weeks apart, is designed to support existing vaccine supplies in the national stockpile.
Disaster News – “The vaccine, manufactured by GlaxoSmithKline, was developed in partnership with the Biomedical Advanced Research and Development Authority, which is under the Office of the Assistant Secretary for Preparedness and Response of the U.S. Department of Health and Human Services.’This vaccine could be used in the event that the H5N1 avian influenza develops the capability to spread efficiently from human to human, resulting in the rapid spread of disease across the glove.’ Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research, said in the news release. Among people who have become infected with H5N1, mortality is about 60%, according to WHO. Health officials have determined the H5N1 strain of influenza has ‘pandemic potential’ because it continues to affect wild birds and poultry populations, and most humans have no immunity to it.”
(image: Bahman Farzad/Flickr)