It’s nearly July, have you signed up for the Summer Workshop on Pandemics, Bioterrorism, and Global Health Security, to get your early registration discount? Also – as you enjoy the summer weather, practice bat safety, as the CDC has warned that they post the biggest rabies threat in the United States.
 How World War II Spurred Vaccine Innovation
How World War II Spurred Vaccine Innovation
Dr. Kendall Hoyt discusses the link between war and disease, and how WWII helped bring forth a renaissance of vaccine development. Did we mention she’ll be speaking at our summer workshop next month? “As the Second World War raged in Europe, the U.S. military recognized that infectious disease was as formidable an enemy as any other they would meet on the battlefield. So they forged a new partnership with industry and academia to develop vaccines for the troops. Vaccines were attractive to the military for the simple reason that they reduced the overall number of sick days for troops more effectively than most therapeutic measures. This partnership generated unprecedented levels of innovation that lasted long after the war was over. As industry and academia began to work with the government in new ways to develop vaccines, they discovered that many of the key barriers to progress were not scientific but organizational.”
Ebola Outbreak – Expanding into Uganda
By June 12th, the Ugandan Ministry of Health had confirmed three cases of Ebola along the DRC border. In many ways, this was the scenario public health officials had been expecting and fearing. “For 10 months, Uganda has closely monitored its porous border with the DRC for crossover cases, yet, despite numerous alerts, no cases have been detected until now. ‘In preparation for a possible imported case during the current outbreak in DRC, Uganda has vaccinated nearly 4,700 health workers in 165 health facilities (including in the facility where the child is being cared for); disease monitoring has been intensified; and health workers trained on recognizing symptoms of the disease. Ebola Treatment Units are in place,’ the WHO regional office for Africa said in a news release.” Given the growth of the outbreak and now cases in Uganda, many are wondering why the WHO has not declared this outbreak a PHEIC (public health emergency of international concern). This may change though, as the WHO Director-General Dr. Tedros has convened an Emergency Committee under the International Health Regulations for Friday (FYI, this is the third time the Emergency committee has met to discuss the outbreak and classification as a PHEIC). Concerns for the delay in declaring PHEIC have been present for months – “The legal criteria for a PHEIC have been met. The International Health Regulations (2005) (IHR) empower the WHO Director-General to declare a PHEIC. A PHEIC is an extraordinary event with public health risk to other countries that requires a coordinated international response. IHR criteria include public health impact, novelty and scale, and movement of persons. The WHO Director-General must also consider health risks, potential international spread, and EC guidance, among other factors.”
Fighting Global Pandemics By Starting One
In the latest video installment from the Bulletin of the Atomic Scientists’s Say What? series, the hot topic of gain-of-function research is being discussed. “Researchers say making new strains of the H5N1 flu virus in a secure lab can help them see what might happen naturally in the real world. Sounds logical, but many scientists oppose it because the facts show most biosafety labs aren’t really secure at all, and experts say the risks of a mutated virus escaping outweigh whatever public health benefit comes from creating them. But now the US government is funding these same labs again to artificially enhance potentially pandemic pathogens. In this installment of the Bulletin’s video series that provides a sharp view of fuzzy policy, Johns Hopkins University computational biologist Steven Salzberg explains why arguments by researchers in favor of risky viral research aren’t persuasive.”
 Burden of Disease Exposures- Reasons to Invest in Hospital Response
Burden of Disease Exposures- Reasons to Invest in Hospital Response
GMU biodefense doctoral student and infection preventionist Saskia Popescu discusses the impact that communicable disease exposures have on hospitals. “The time spent responding to an exposure means less time for patient care and infection prevention, but can also result in health care workers having to stay home if they’re exposed and immuno-naïve. A new survey sought to understand the impact for infection preventionist and staff nurses when an exposure to a communicable disease occurs. Investigators wrote in the American Journal of Infection Control (AJIC) regarding this very issue and surveyed staff nurses in a New York hospital network and infection preventionists at the 2018 Association for Professionals in Infection Control and Epidemiology annual conference, as well as members of the Association for Professionals in Infection Control and Epidemiology chapters. A total of 150 nurses and 228 infection preventionists responded with some insight into just how time-consuming these exposures are. Data regarding workload increase for each exposure was captured in 2 questions asking participants to rank the overall increase in daily workload for each of these exposures (0-3 scale, with 0 meaning not applicable and 3 meaning a dramatic increase in workload of more than 60 minutes), and to explain the 3 most time-consuming activities for outbreak and exposure activities. Infection preventionists reported the most time-consuming outbreaks/exposures resulted from mumps/measles, tuberculosis, gastrointestinal viruses, and multidrug-resistant organisms. For an exposure to Clostridioides difficile, lice or scabies, and influenza, there was a more than 60-minute workload increase for nurses.”
There’s Limited Time To Make America Safer From Epidemics
Dr. Tom Frieden and Margaret Hamburg shine a light on a harsh truth – we’re on tight window if we want to avoid a pandemic. “In one week, the World Bank will decide how to allocate more than $50 billion in development funding to lower income countries. The World Bank should dedicate some of its International Development Association (IDA) funds – say, 5 percent, or about $1 billion per year over three years – to help countries become better prepared for infectious disease outbreaks.” “Disease outbreaks can wipe out years of investments and severely damage development. Economic losses can dwarf the cost of response – the World Bank estimates that SARS cost the global economy $54 billion in little over half a year and that a severe flu pandemic could cost more than $3 trillion, nearly five percent of global GDP. Because of its global reach, the World Bank is in the best position to take the lead on this critical effort, but the United States delegation has one week to make sure it does so at its annual meeting on June 17. The total needed to close preparedness gaps is estimated at about $4.5 billion annually, less than $1 per person per year. An additional $1 billion infusion each year for the next three years will provide a tremendous jump start – and is a bargain the United States cannot afford to miss.”
Russian Biologist Plans for More CRISPR Babies
Just went you thought the CRISPR baby drama was over (or at least being managed)…. “A Russian scientist says he is planning to produce gene-edited babies, an act that would make him only the second person known to have done this. It would also fly in the face of the scientific consensus that such experiments should be banned until an international ethical framework has agreed on the circumstances and safety measures that would justify them. Molecular biologist Denis Rebrikov has told Nature he is considering implanting gene-edited embryos into women, possibly before the end of the year if he can get approval by then. Chinese scientist He Jiankui prompted an international outcry when he announced last Novemberthat he had made the world’s first gene-edited babies — twin girls. The experiment will target the same gene, called CCR5, that He did, but Rebrikov claims his technique will offer greater benefits, pose fewer risks and be more ethically justifiable and acceptable to the public. Rebrikov plans to disable the gene, which encodes a protein that allows HIV to enter cells, in embryos that will be implanted into HIV-positive mothers, reducing the risk of them passing on the virus to the baby in utero. By contrast, He modified the gene in embryos created from fathers with HIV, which many geneticists said provided little clinical benefit because the risk of a father passing on HIV to his children is minimal.”
Stories You May Have Missed:
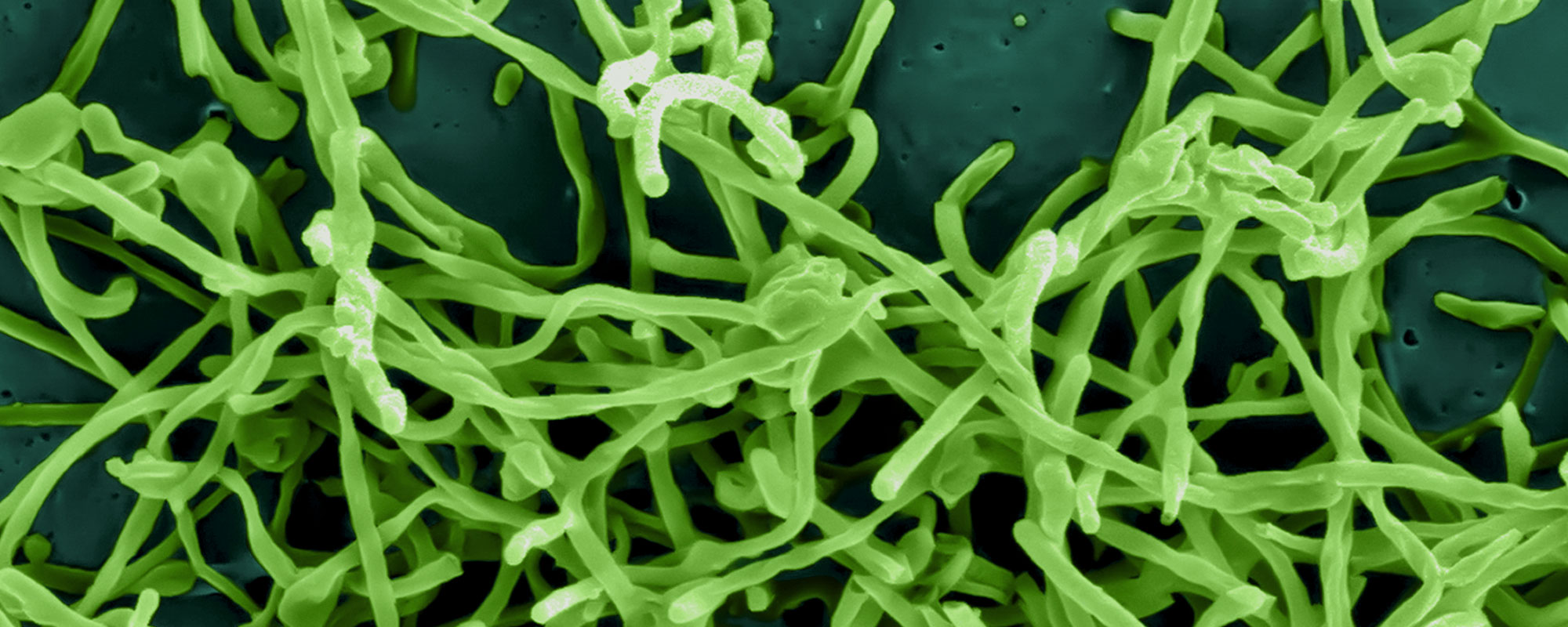
- Microbial House Designs– “There’s a little mischievousness about bringing all these things and making them visible,” said Mr. Pallrand’s wife, Rachel Mayeri, who based the tile designs on electron microscopy images. “These things we tend to think of as being kind of ugly and want to hide — mold spores and mildew growing in our bathtub, and bacterial colonies that are on all the surfaces of your house — they’re all noncharismatic animals, but they’re really crucial to our lives.”





 We’re also excited to announce the following Biodefense MS graduates – Zamawang Almemar, Mariam Awad, Laramie Bradford, Michael Conway, Alexander Dowsett, Sarah Doyle, Stephanie Ellis, Haziq Ghani, Zachary Goble, Stephanie Kiesel, Alexander Rowe, Stephanie Smith, and Alexandra Williams. We’d also like to congratulate three of our biodefense graduate students for their student achievements – Stephanie Smith (Outstanding Biodefense Student), Saskia Popescu (Frances Harbour Award- Biodefense Community Leadership), and Christopher Brown (Outstanding Doctoral Student in Biodefense).
We’re also excited to announce the following Biodefense MS graduates – Zamawang Almemar, Mariam Awad, Laramie Bradford, Michael Conway, Alexander Dowsett, Sarah Doyle, Stephanie Ellis, Haziq Ghani, Zachary Goble, Stephanie Kiesel, Alexander Rowe, Stephanie Smith, and Alexandra Williams. We’d also like to congratulate three of our biodefense graduate students for their student achievements – Stephanie Smith (Outstanding Biodefense Student), Saskia Popescu (Frances Harbour Award- Biodefense Community Leadership), and Christopher Brown (Outstanding Doctoral Student in Biodefense).





